


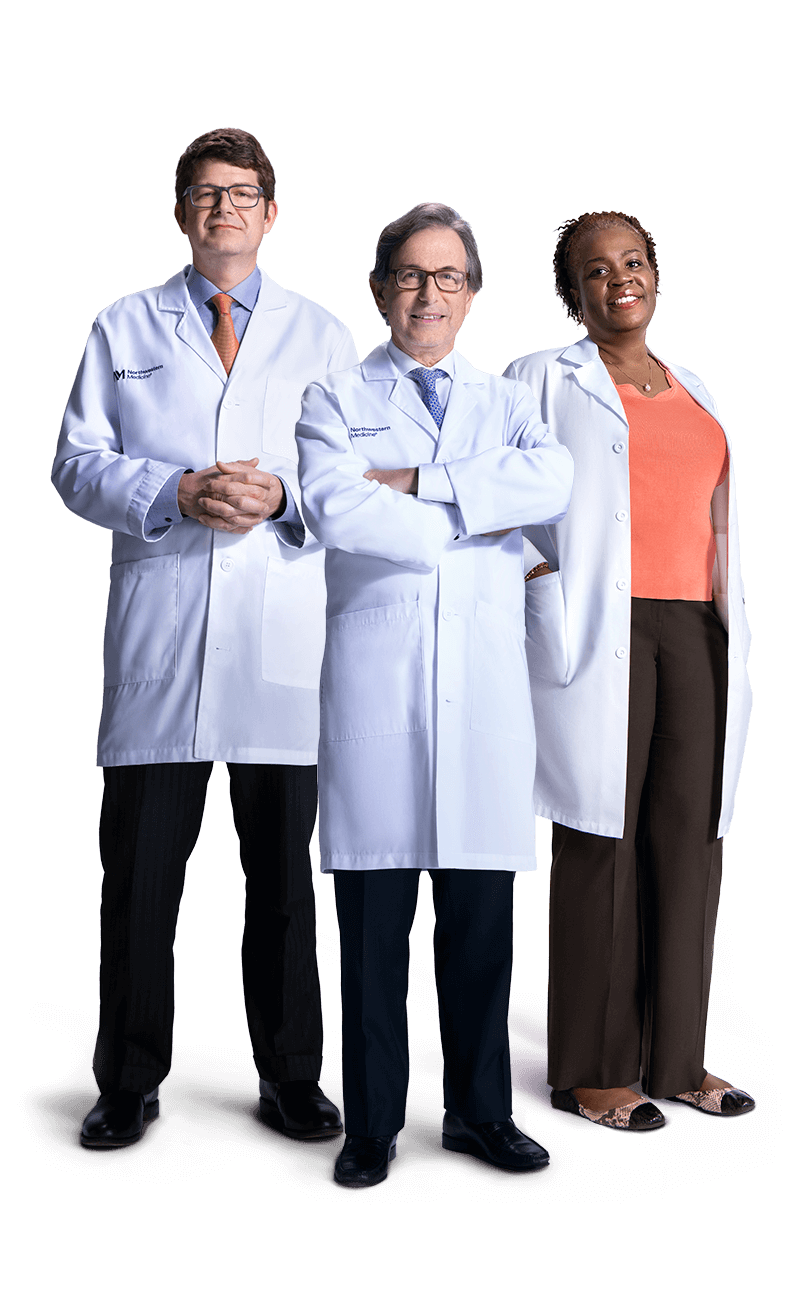

A ONE IN A MILLION TEAM
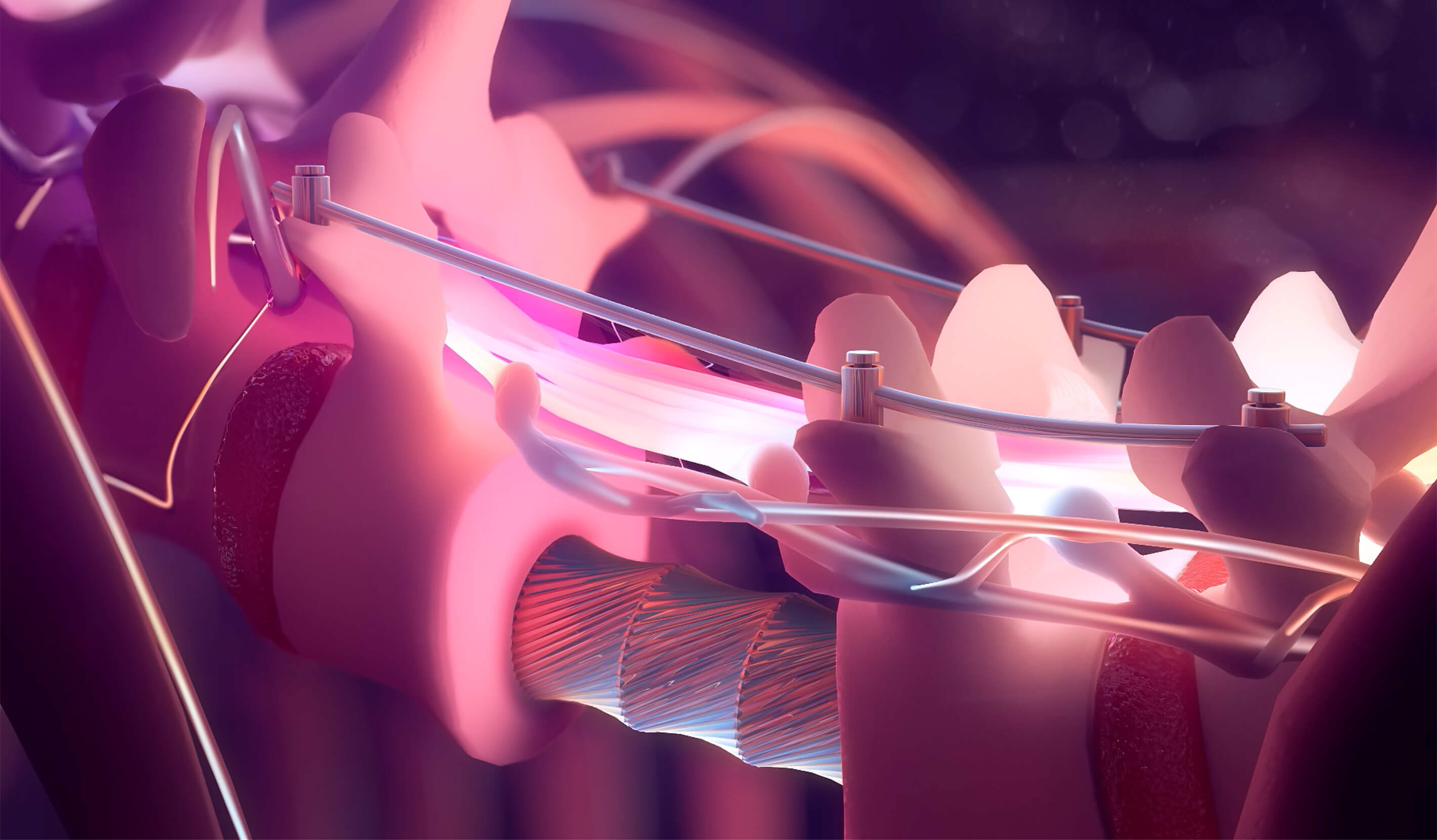
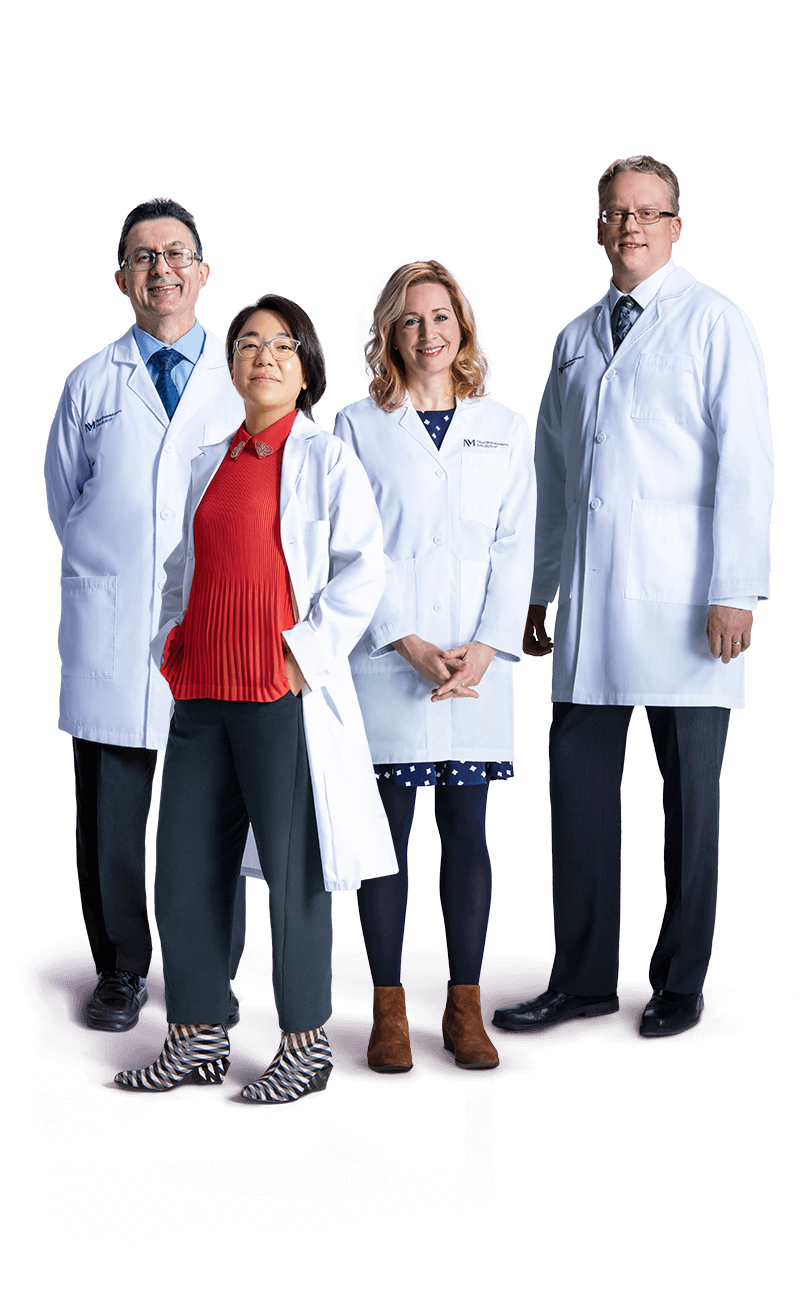
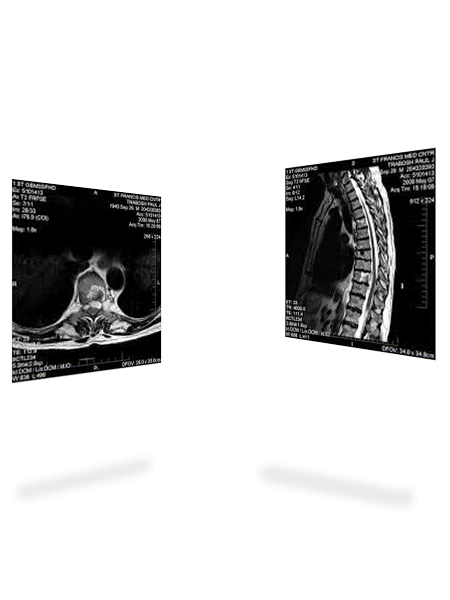
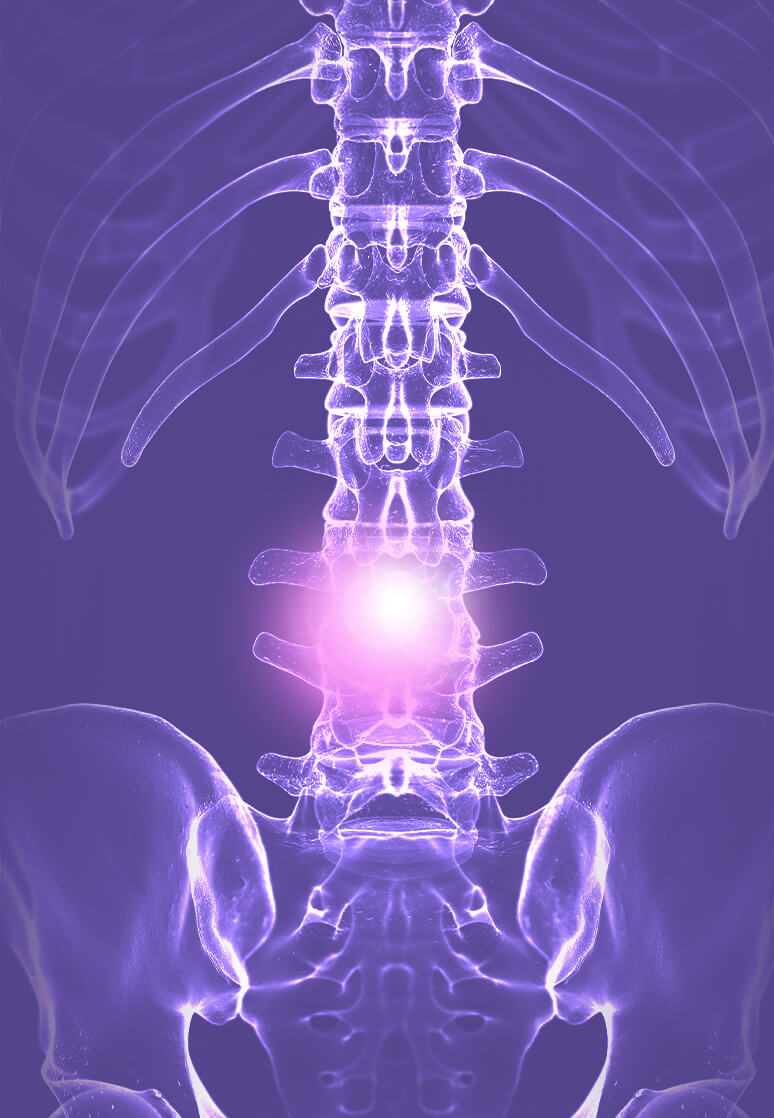
When internationally renowned neurosurgeon Jean-Paul Wolinsky, MD, joined the Lou and Jean Malnati Brain Tumor Institute of the Robert H. Lurie Comprehensive Cancer Center of Northwestern University at Northwestern Memorial Hospital in 2017, it was precisely for a procedure like this. As chordomas only occur in one out of a million people, finding a care team with experience removing one can be difficult. But Dr. Wolinsky would come to find that his new colleagues not only suited his objective; they exceeded his expectations entirely.
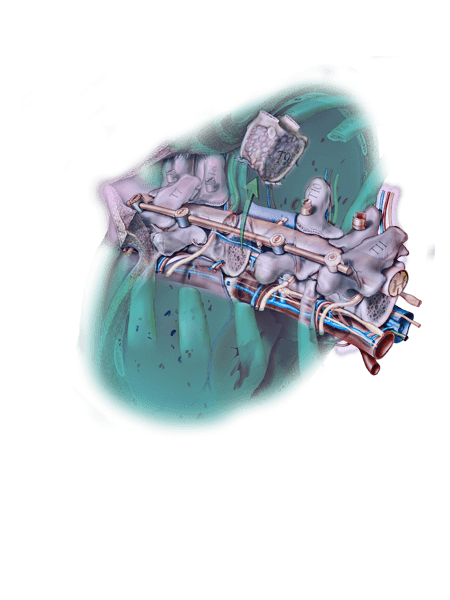
The depth of clinical expertise at Northwestern Memorial Hospital is hard to match. Nearly 30 surgeons, along with supporting staff, consulted on Jeff’s chordoma removal.




What makes us better, makes you better.®
LEADING BY EXAMPLE
At any given time, fewer than one in 100,000 people worldwide may be living with a chordoma. But throughout the Northwestern Medicine system, preparedness to treat any patient with any illness is core to the mission.
I think that is what’s invigorating about something like the tumor board, having the opportunity to spar with top-tier colleagues to improve or pioneer the best possible outcomes for our patients. You’ve gotta bring your A game.
With his colleagues, Dr. Wolinsky continues to explore new opportunities for chordoma treatment, from utilizing 3-D printed bones as a potential substitute for titanium reconstruction to continued advances in proton therapy and the use of novel drug therapies. Though chordomas may be rare in the general population, they are not rare to the Northwestern Medicine specialists paving the way for better outcomes for patients.