Better Urology for Gay and Bisexual Men
How One Program Is Helping Heal a Community
Published May 2022
During his residency, Northwestern Medicine Urologist Channa Amarasekera, MD, noticed that some patients were being overlooked during their urological care. He knew that needed to change.
Those patients were men who identified as gay or bisexual, and/or men who have sex with men (MSM). And now Dr. Amarasekera is the director of the Northwestern Medicine Gay and Bisexual Men's Urology Program — the first of its kind in the United States. The program was launched in August 2021 and sees patients in two locations: in downtown Chicago and in Northalsted, a neighborhood in Chicago with a large population of gay and bisexual men.
We're changing the narrative. We are here to help.— Channa Amarasekera, MD
According to Dr. Amarasekera, care teams typically counsel and treat men under the assumption that they do not have sex with other men. However, MSM may have different urological concerns and priorities than men who do not have sex with men. For example, erectile and sexual function in relation to the prostate may be a key health focus for these patients, Dr. Amarasekera explains.
"There has been a big blind spot in medical education when it comes to MSM and other LGBTQ populations," he says. "With this program, we're really trying to end those distressing experiences for the patients we serve."
Medical professionals in the Gay and Bisexual Men's Urology Program take a mindful approach to the urologic care experience for patients who were assigned male at birth (AMAB) and who identify as gay or bisexual, and/or who choose to have sex with men.
Conducting Research
After he noticed gay and bisexual patients were not getting the comprehensive urologic care they needed, Dr. Amarasekera began researching what led to these disappointing care experiences and how physicians could offer better care. He found that MSM, as well as transgender and other sexual and gender minority patients, had unmet health needs.
Additionally, patients now in the recommended age range for prostate cancer screening lived through the HIV/AIDS crisis in the 1980s and may have witnessed a general negligence of the medical needs of sexual minorities, Dr. Amarasekera explains. As a result, LGBTQ people who grew up during the worst of the crisis may have a lingering distrust of medical institutions.
"LGBTQ health has been largely underfunded and underserved," Dr. Amarasekera says. "We're changing the narrative. We are here to help."
Addressing Gaps
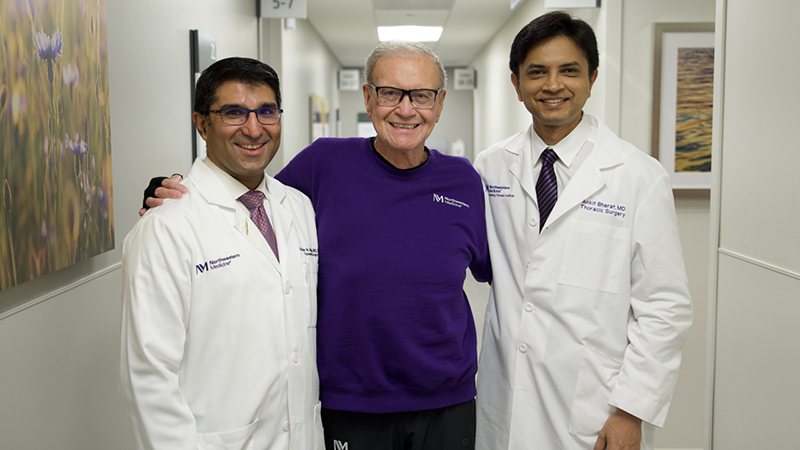
Under Dr. Amarasekera's leadership, care teams are committed to fully understanding who, where and how their patients are because those details influence treatment decisions. This comprehensive and trusting approach to patient care is improving the lives of LGBTQ patients and families in the Gay and Bisexual Men's Urology Program.
"We're working to identify what's important to the patients, what's working for them and what's not," Dr. Amarasekera says. "We're thrilled to be able to learn from our patients about how best to serve them."