Eczema or Hives?
How to Tell the Difference Between the Skin Conditions, Plus Treatment Options
Published July 2025
Itchy and disruptive, eczema and hives can negatively impact your quality of life. While both of these common skin conditions are types of rashes and neither is contagious, they have different underlying causes, durations, appearances and treatment approaches. Fortunately, advancements in treatment and diagnostic tools are helping people find relief and regain control of their skin health.
Eczema is not due to food allergies.— Walter J. Liszewski, MD
Major Differences Between Eczema and Hives
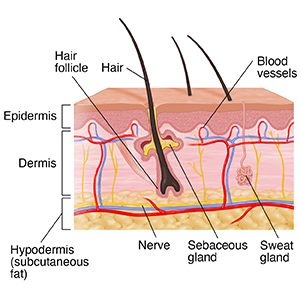
Eczema occurs when the top layer of the skin (the epidermis) becomes damaged or inflamed. This can be due to genetic predisposition, non-food allergies or exposure to irritating chemicals. Atopic dermatitis is the most common form.
Hives (urticaria) are caused by inflammation deeper in the skin, known as the dermis. Hives form when certain cells in your skin release histamine, a chemical that causes small blood vessels to leak fluid under your skin. This can be caused by allergens or non-allergic triggers, such as stress or heat.
"Eczema affects the outer layer of the skin, while hives involve inflammation deeper in the dermis," explains Walter J. Liszewski, MD, a dermatologist at Northwestern Medicine.
Additional key differences include:
Symptoms and Appearance
- Eczema: Dry, flaky red patches that may ooze or crust over
- Hives: Raised, red or skin-colored welts that may appear suddenly and itch or burn
Common Triggers
- Eczema: Makeup, sunscreen, lotions, soaps, detergents, jewelry, adhesives and certain fabrics like wool, polyester and nylon
- Hives: Pollen, pet dander, foods, insect stings, stress and heat
"Makeup allergies can cause eczema but not hives," explains Dr. Liszewski. "Hives are more likely to be caused by things like bees, grass, pollen, cats, dogs or food.” He adds, “Eczema is not due to food allergies.”
Location
- Eczema: Commonly affects the hands, face, neck, elbows and knees
- Hives: Can appear anywhere on the body and often move around
Duration
- Eczema: Can be chronic and long-lasting, with flare-ups over time
- Hives: May last hours to days if acute, or six weeks or longer if chronic
Diagnosing Eczema and Hives
To figure out the cause of eczema or hives, clinicians may use allergy testing. There are two main types:
- Patch testing involves placing small amounts of potential allergens on the skin, usually on the back, and monitoring for reactions over several days. This method is used to show delayed allergic reactions, which are more common in eczema.
"We use patch testing to identify allergens that cause eczema," says Dr. Liszewski. "We apply 100 to 150 chemicals to a patient’s back and monitor which ones cause a reaction. Then we review their personal care products and create a treatment plan that avoids those allergens."
- Prick testing involves pricking the skin with a small amount of an allergen to evaluate immediate allergic reactions, which are more typical in hives.
"Prick testing is used to evaluate immediate allergies like food, pollen or pet dander,” says Dr. Liszewski.
If you are on a medication that may interfere with patch or prick testing, or you can’t tolerate skin testing, your physician may order an allergy blood test that measures antibodies in your blood in response to specific allergens.
Treatment Options
Treatment for eczema and hives depends on how severe the symptoms are and what’s causing them. “The best thing is to treat the underlying inflammation,” says Dr. Liszewski.
Treatments for Eczema
- Moisturize regularly, especially after bathing when your skin is damp, to help repair your skin barrier. This outermost layer of skin helps maintain hydration and protects against allergens and irritants.
- Use topical steroids to reduce inflammation and repair your skin barrier.
- For more moderate to severe eczema, your physician may recommend taking:
- Oral immunosuppressant medication, which broadly suppresses your immune system and reduces inflammation
- Biologic medication, which targets specific parts of your immune system involved with eczema
In 2024 and 2025, the Food and Drug Administration (FDA) approved multiple injectable biologic medications for the treatment of eczema and chronic hives:
- Nemolizumab-ilto (Nemuvio®): approved for both eczema and chronic hives
- Lebrikizumab-lbkz (Ebglyss®): approved for eczema
- Lebrikizumab-lbkz (Ebglyss®): approved for eczema
These medications target the underlying source of inflammation inside the body and have been shown to reduce itching.
“For atopic dermatitis, we now have an abundance of options to offer patients,” says Dr. Liszewski. “If someone is struggling with moderate to severe eczema, there’s a lot we can do for them that doesn’t involve topical steroids.”
Treatments for Hives
- Oral antihistamines (a first-line treatment)
- Topical steroids to reduce inflammation and repair your skin barrier
For people with chronic hives who don’t respond to antihistamines or topical steroids, biologic medications or oral steroids may be prescribed to help reduce inflammation, itching and hive activity.
“We tailor treatment plans to each patient’s needs,” says Dr. Liszewski. “For some, it’s about avoiding allergens. For others, it may involve advanced therapies like biologics or immunomodulators.”
When to Seek Care
If you experience persistent itching, redness or swelling, it’s important to see a medical professional. Early diagnosis and treatment can prevent symptoms from worsening and improve your quality of life.
It’s helpful for your physician to know when your rash occurs and any recent changes in your habits, like using a new hair care product or laundry detergent. Be sure to document and share this information at your appointment.