Breaking Barriers in Brain Tumor Treatment
Ultrasound Device Breaks Blood-Brain Barrier to Deliver Chemotherapy and Immunotherapy to Brain Tumors
Updated May 2024
This article was originally published in the Northwestern University Feinberg School of Medicine News Center. It has been edited for the HealthBeat audience.
In 2023, physicians at Northwestern Medicine made an important discovery in the treatment of brain cancer. Using a special device with ultrasound technology developed in France by a company called Carthera, they can deliver powerful chemotherapy medications directly to aggressive brain tumors. Normally, these medications can’t reach the tumors because of a protective barrier called the blood-brain barrier. The barrier is a collection of cells and structures that helps prevent bacteria, fungi, viruses, parasites and other intruders from reaching the brain.
This is potentially a huge advance for patients with glioblastoma.— Adam M. Sonabend, MD
In the first human clinical trial, published in The Lancet Oncology in 2023, researchers placed an ultrasound device in the skull to temporarily open the blood-brain barrier. With the implanted device in place, researchers inject microscopic gas bubbles into the bloodstream as the ultrasound starts. The ultrasound waves cause these bubbles to vibrate (sonication), weakening the blood-brain barrier to let medication pass through. Researchers found that when the blood-brain barrier was opened, the concentration of the chemotherapy medication in the brain increases by about four to six times.
The brain sonication procedure done with this implant is about a four-minute process that is performed with the patient awake. Patients can go home after a few hours. Results of the clinical trial show the treatment is safe and well tolerated, with some patients getting up to six cycles of the treatment.
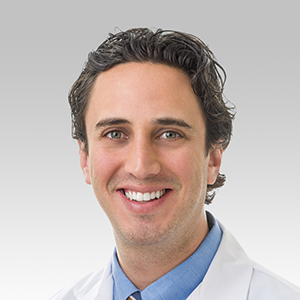
“This is potentially a huge advance for patients with glioblastoma,” says Lead Investigator Adam M. Sonabend MD, a neurosurgeon at Northwestern Medicine and associate professor of Neurological Surgery at the Northwestern University Feinberg School of Medicine. He adds that temozolomide, the current chemotherapy used for glioblastoma, is one of the few that crosses the blood-brain barrier, but it is a weak medication. With the ultrasound device, care teams can use more powerful chemotherapy medications.
Dr. Sonabend works alongside Roger Stupp, MD, neuro-oncologist and co-director of Lou and Jean Malnati Brain Tumor Institute of Robert H. Lurie Comprehensive Cancer Center of Northwestern University. They collaborated on this and other clinical trials on the human brain.
A Second Discovery
During the clinical trial, researchers also discovered that the blood-brain barrier closed again after about an hour, which is shorter than what previous studies found. This knowledge helps with the timing of medication sequencing, delivery and penetration.
Researchers are now conducting a phase 2 clinical trial for patients with recurrent glioblastoma to see if this treatment can help them live longer. They also opened another clinical trial using this same technology to deliver immunotherapy to the brain to treat newly diagnosed glioblastoma. If successful, the approach also could be used to develop treatment for other brain diseases.
“While we have focused on brain cancer, for which there are approximately 30,000 gliomas in the U.S., this opens the door to investigate novel drug-based treatments for millions of patients who have various brain diseases,” says Dr. Sonabend.
Learn more about clinical trials and research.