Rehabilitation Helps Physician Find the Right Words After a Stroke
Northwestern Medicine Aphasia Center Improves Language and Communication Skills
Published August 2023
Just days after surviving a stroke Eric Werner, MD, walked out of Northwestern Medicine Central DuPage Hospital unassisted. However, while he was doing well physically, the 62-year-old was experiencing an invisible impact of stroke — aphasia. Aphasia is a language disorder, most often caused by strokes, that affects a person’s ability to communicate.
Aphasia can affect a person’s ability to speak, understand what they hear, read, and write. There are several different types of aphasia that can be acquired based on where the stroke happened in the brain. People can also experience aphasia to varying degrees of severity.
Dr. Werner’s Story
Last June, Dr. Werner, an anesthesiologist at Northwestern Medicine, was alone at his St. Charles, Illinois, home when he dropped to the ground. Too weak to stand, he couldn’t reach his phone. As he fell in and out of consciousness, he couldn’t comprehend exactly what was happening.
Aphasia may not completely resolve, but patients can make amazing progress.— Michelle Armour, MS, CCC-SLP
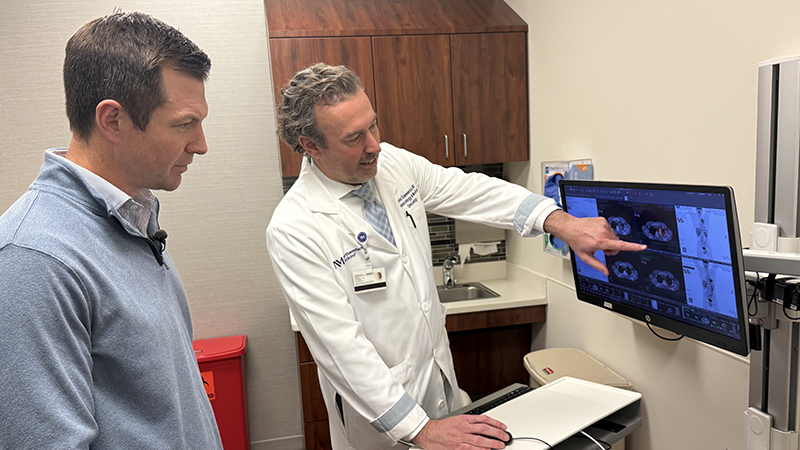
About two hours later, Dr. Werner’s wife returned home and immediately called 911. He received advanced treatment in the Northwestern Medicine Mobile Stroke Unit, an ambulance equipped with a 16-slice CT scanner and stroke medications to start stroke intervention earlier. Stroke intervention is most effective within three hours of when the stroke has occurred. He was rushed to the Interventional Lab at Northwestern Medicine Central DuPage Hospital to remove a blood clot in his brain that was causing the stroke.
“With the Mobile Stroke Unit, we can take the hospital to the patient and provide treatment right away in the field,” says Harish Shownkeen, MD, medical director of the Stroke and Neurointerventional Surgery Programs at Central DuPage Hospital. “This early intervention leads to better outcomes, as every second counts when you are treating a stroke.”
Dr. Werner was out of his hospital bed and walking the next day. Within a week, he was discharged and went home.
“It felt like a miraculous recovery,” says Dr. Werner.
Regaining the Ability to Communicate
However, while he felt great physically, Dr. Werner was having trouble verbally expressing what he was thinking, as well as distinguishing what he was hearing. For example, he would mix up certain letter combinations, such as a “th” and “sh,” making it difficult to understand words. He was diagnosed with aphasia.
“Aphasia results from damage to the language center of the brain. Intellectual skills are perfectly intact, but there is a disruption in the ability to communicate,” says Michelle Armour, MS, CCC-SLP, program lead clinician of the Northwestern Medicine Aphasia Center at Marianjoy Rehabilitation Hospital. “Aphasia may impact listening, speaking, reading and writing. Every individual is different, so not everyone experiences changes in all of these areas.”
To improve his functional communication and language, Dr. Werner attended outpatient skilled speech-language therapy at Northwestern Medicine Marianjoy Rehabilitation Hospital. Typical therapies for aphasia include:
- Restorative therapies are aimed at improving or restoring function
- Compensatory therapies are aimed at compensating for the difficulty in communicating.
Therapy aims to address both:
- Receptive language: the ability to understand and comprehend spoken language that you hear or read
- Expressive language: the ability to express your wants and needs through verbal or nonverbal communication
“With Dr. Werner, we specifically focused on verbal expression, thought organization, auditory processing and motor speech skills,” says Amy Nourie, MA, CCC-SLP, speech-language pathologist at Marianjoy. “Dr. Werner demonstrated exceptional effort and follow-through by completing home exercise programs, which positively affected his success of recovery.”
The goal is to stimulate the brain’s language center to engage aspects of neuroplasticity, the ability of the nervous system to change by reorganizing its structure, functions or connections after injuries, such as a stroke or traumatic brain injury. Patients also learn new methods of communication, such as gestures, pictures or the use of electronic devices.
Putting in the Work
“At first the recovery is remarkable, but then it slows down and over the next year there is a gradual improvement,” Dr. Werner says. “I’ve faced this like a mountain to climb. If I feel like I’m hitting a wall, I try something new. Recovery has become a full-time job.”
In addition to outpatient treatment, Dr. Werner attended an eight-week group program at the Aphasia Center at Marianjoy. In a small-group setting, participants practice communicating through real-life activities including conversation, games, math, writing, music, technology and book clubs. Each session focuses on improved language functioning, increased socialization, independence and improved quality of life.
Dr. Werner made new friends at the Aphasia Center and feels one of the biggest advantages of the group setting is the social interaction.
“People with stroke tend to self-isolate,” says Dr. Werner. “I’ve made a big effort to not do that with my friends. The more opportunities I have to speak with others, the better. People are very supportive and understanding.”
Today, Dr. Werner’s aphasia is rarely apparent to others. But Dr. Werner is very aware of the extra work he must do, especially during fast-paced conversations. With enthusiasm and optimism, he continues to look forward and is dedicated to working on his speech several hours a day.
“For some patients, aphasia may not completely resolve,” Armour says, “but they can make amazing progress, for the rest of their life, as they continue to practice their skills.”