Is There More to Varicose Veins Than Meets the Eye?
Get the Full Picture
Published September 2025
Those swollen veins that you can see just under the surface of the skin are varicose veins. They often have a twisted appearance and blueish-purple color tone. You may notice them in your legs, ankles and feet. They can also show up in your arms and pelvic area, but it’s less common than in your legs. That’s because your leg veins are under more strain while standing and walking.
Varicose comes from the Latin word that means ‘worms.’— Scott A. Resnick, MD
While varicose veins may be easy to spot, they’re not always easy to understand. You might wonder:
- Why do you develop varicose veins?
- When should you talk to your doctor about them?
- What are the treatment options?
- Can you prevent varicose veins?
Scott A. Resnick, MD, a vascular and interventional radiology physician at Northwestern Medicine, answers these questions and more with a closer look at the anatomy of varicose veins.
The Vein Network
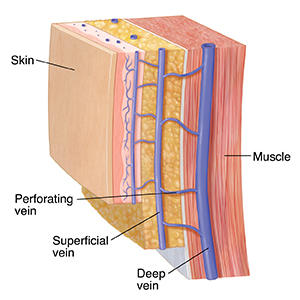
There are two vein systems in your legs: deep veins and superficial veins (the veins closer to the skin). Your perforating veins carry blood from the superficial veins to the deep veins.
“Both systems do the same thing — they carry blood from the leg up and out, back to the body, back to the heart, to move the blood around,” says Dr. Resnick. “This is a challenge because it’s uphill and against gravity. The superficial veins have a harder job because they work with valves rather than with the help of our leg muscles. This is where varicose veins can form.”
- Deep veins work along the musculature system and carry most of the blood flow. Blood flow is activated by leg muscles, mostly the calf muscle, by walking and flexing your foot at the ankle.
- Superficial veins carry only 10% to 15% of the blood flow, using one-way valves outside of the muscular pump.
If gravity pulls blood backward, valves in the superficial vein system may leak. This can lead to varicose veins.
How Varicose Veins Form
“Varicose comes from the Latin word that means ‘worms,’” says Dr. Resnick. “Varicose veins are caused by a variety of different reasons. By far the most common is something we call venous insufficiency, which is leaky valves within certain veins in our legs.”
Leaky valves in the superficial vein system are very common. When they don’t work properly, blood can flow backward. Not everyone with leaky valves will develop varicose veins; the veins only become varicose when they dilate or stretch to make room for the extra blood volume.
“If we were to randomly pull people off the street and scan them, somewhere around 10% of men and 20% of women would have leaky valves,” adds Dr. Resnick. “Now, many of them would have no signs or symptoms. There are reasons why some people are at greater risk for varicose veins.”
Risk Factors for Varicose Veins
- Family history
- Excess weight or changes in weight
- Older age
- Hormone changes (people who are pregnant, menopausal, or taking hormone replacement or contraceptive medications are at higher risk)
- Being inactive (standing or sitting for long periods of time)
- Leg injury or trauma
- Smoking
Symptoms of Varicose Veins
When a varicose vein stretches your vein wall, it can lead to tension and blood flow changes. This can trigger symptoms like:
- Visible, bulging veins
- Swelling in the legs, especially in the ankles and calves
- Skin changes, such as discoloration, dryness, sores or rash
- Itching by the varicose vein
- Pain or cramping in your legs
How to Prevent Varicose Veins
You can’t always prevent them, especially as you get older or if you have a family history. However, there are several self-care tips you can follow to help manage and slow down varicose veins from getting worse:
- Stay active and move often (helps push blood upward)
- Keep a healthy weight
- Avoid standing or sitting for long periods without changing your position
- Elevate your legs above your heart three to four times a day for about 15 minutes at a time
- Wear compression stockings
- Eat a high-fiber, low-salt diet and stay hydrated
What about spider veins?
Spider veins are generally tiny, thin red, blue or purple veins right below the skin surface that are either flat or only a little bit bulging. Varicose veins tend to be larger and bulge more clearly.
“Spider veins are not related to valve problems and are much more common in women,” says Dr. Resnick. “While they are symptom-free and often considered cosmetic problems in the eyes of insurance carriers, some patients do have symptoms related to spider veins, including itching and burning and a sensation of warmth. A small percentage may even experience bleeding.”
Health Risks of Varicose Veins
Skin problems. “The change of skin color in and of itself is not a problem. But it’s a sign of how far down the path you’ve progressed. And it gets our attention,” says Dr. Resnick. “If it’s not treated, it may not get any worse. For others, it may develop into a chronic inflammatory skin condition called lipodermatosclerosis.”
This condition is often associated with chronic venous insufficiency. It can make the skin around the ankles or calves become reddish or purple and feel hard. In severe cases, open skin or ulcers may develop.
Blood clots. Having varicose veins may increase your risk of developing blood clots. Unlike deep vein thrombosis (DVT) where blood clots form in the deep veins of the legs, superficial blood clots or superficial vein thrombosis (SVT) from varicose veins do not usually travel to the lung. Please know that DVT is a serious condition and if you have severe varicose veins, it’s important to talk to your doctor to know your risk.
Treatment for Varicose Veins
When varicose veins impact your quality of life, Dr. Resnick recommends seeing a specialist. The evaluation usually involves a short consultation with an ultrasound, which takes about 30 minutes for each leg.
The treatments are becoming easier to tolerate, too.
“In the past, there was what we called vein stripping. It’s surgical procedure with general anesthetic where the varicose veins were surgically stripped, removed from the body,” says Dr. Resnick. “That was effective but quite an undertaking. Today, the modern therapies involve similar outcomes in a less invasive manner.”
More common, less-invasive procedures to treat varicose veins are generally done in a clinic using a local anesthetic without sedation. These include:
- Sclerotherapy. A chemical is injected into the affected vein. The chemical causes scarring in the vein so that it can no longer carry blood. Sclerotherapy is also used to treat spider veins.
- Thermal ablation. A laser puts heat into the affected vein and closes it.
- Ambulatory phlebectomy or microphlebectomy. A special hook is used to gently take out a varicose vein through tiny incisions.
Managing varicose veins can feel challenging. But finding relief and treatment doesn’t have to be.