Diagnosis
Diagnosis of Melanoma
Melanoma care with Northwestern Medicine Dermatology
Diagnosis
Early diagnosis of melanoma is one of the most important factors for successful treatment and improved survival. To achieve this, our physicians use innovative techniques such as dermoscopy, digital automated total body mole mapping and short-term dermoscopic monitoring.
Dermoscopy
What is it?
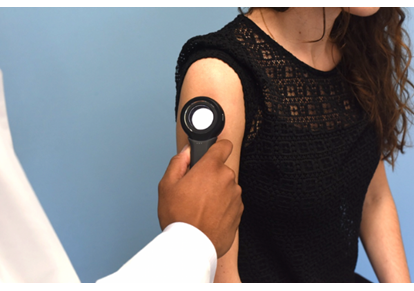
Dermoscopy involves using a specialized handheld device with a magnifying lens and a special polarized light. It allows clinicians to see the deeper layers of skin that are not visible to the naked eye.
Why do we use it?
Dermoscopy is about nine times more sensitive in detecting melanoma than the naked eye.1 It also significantly reduces unnecessary biopsies, by as much as 42%.1 Dermoscopy allows the physician to detect subtle characteristics of melanoma, confidently rule out benign lesions and decide whether a biopsy is needed. Dermoscopic images can also be taken for close observation of borderline lesions. Northwestern Medicine Dermatology leads several local and national educational and research programs on dermoscopy, including a dermoscopy course for the American Academy of Dermatology for the past three years. The team has also organized and hosted a dermoscopy lecture series, which is currently available to view on-demand on our virtual event hub.
Digital automated total body mole mapping

What is it?
Our physicians use the latest technology to detect early melanoma and do surveillance for high-risk patients. This is especially helpful for patients with a large number of moles. During total body imaging, (the pictures are not taken by the clinician) pictures of the entire skin surface while the patient stands in different positions. These images are then stored in a secure online portal. Our melanoma specialists can then access them during follow-up visits.
Why do we use it?
The smart digital automated software can help your clinician identify lesions needing a biopsy. It allows them to compare new images with previously stored ones. Lesions greater than two millimeters undergo lesional registration. Once there are at least two sets of pictures, the software detects subtle changes in size, color, and/or symmetry of existing moles. It also detects new spots. This helps detect melanoma at its earliest stage. The device also has a built-in dermatoscope camera. Your clinician can use this to photograph suspicious lesions for closer monitoring.
Genetic Testing
Although most melanomas occur sporadically, some people are born with an increased risk of developing a melanoma. Melanoma can run in families. This occurs when certain genes have mutations that are carried from one generation to the next. These cases of melanoma are known as hereditary melanoma syndromes.
Our clinic offers testing for patients who have a family history of melanoma developing at a young age. For these patients, we offer genetic screening and counseling. This form of testing involves collecting a sample of your saliva and screening for several genes. We accept referrals from outside dermatologists, too. If any mutations are detected, your dermatologist will discuss the results and next steps with you.
Your dermatologist may consider these factors when deciding on screening:
- Multiple melanomas or melanomas in several relatives
- History of other cancers including, but not limited to, pancreatic cancer, kidney cancer or mesothelioma in close relatives
- History of a relative with a known gene mutation that increases the risk of melanoma
Biopsy
Once your physician identifies a suspicious mole, they may do a biopsy. They do this to remove most or all of the lesion. This allows for a dermatopathologist to examine it under a microscope and give a definitive diagnosis. If they diagnose it as melanoma, they will also perform tumor staging.
