Understanding Pain
Understanding Pain
The International Association for the Study of Pain (IASP)* defines pain as: an unpleasant sensory and/or emotional experience associated with actual or potential tissue damage or described in term of such damage.
The sensation of pain is generated by nerves that send signals to the brain letting it know organs or tissues are damaged or irritated. The brain then sends signals to these organs or muscles to take appropriate action. In medical terms, pain is divided into two categories:
- Acute pain: This type of pain is temporary, and goes away quickly. It is very useful because it lets your body know that something is damaged and to protect it so that you can heal. It is similar to having a cut and avoiding touch in order to let it heal.
- Chronic pain: This is pain that is unpleasant and lasts for prolonged periods of time. It may occur after having acute pain onset. It is usually described as chronic if you have had pain in the same location for greater than three to six months. This type of pain is not useful because it may persist for long periods of time without evidence of further injury. It does not act as a warning system but may lead to depression, despair, helplessness and loss of function.
Learn more about types of pain.
Treatment of pain
The treatment of pain begins with an assessment of the severity of pain and the extent of any injury that may be present. This may include an extensive neurologic and/or musculoskeletal exam. It may involve imaging tests to make sure there are no potentially serious causes for one’s pain. Initial treatment is usually conservative, including heat, cold, ice and over–the–counter medications.
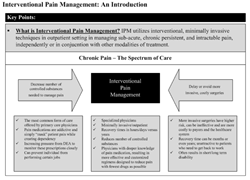
The next step in the treatment of pain is a combination of physical therapy and/or prescription pain medications. Many times, it is necessary to have an interventional pain management procedure done to address acute pain so that one can effectively participate in physical therapy.
If prescription pain medication and physical therapy do not work, the next step may be interventional pain management. If one had sudden loss of function or has neurological deficits, surgical management is indicated.
If interventional pain management does not alleviate the pain, surgery might be required. Even after surgery, however, interventional pain management has a very important role in the treatment of patients’ pain especially when all other options have failed.
Effects of pain
Chronic pain is estimated to cost the U.S. Economy $100 Billion annually.- Back pain is the leading cause of disability in Americans under age 45
- 36 million Americans missed work in the previous year due to pain
- 83 million Americans indicated that pain affects their participation in various activities
Pain statistics
- 76.5 million people in the U.S. age 20 and older are affected by chronic pain (26 percent of the population)
- An estimated 80 percent of all Americans will experience some form of back pain during their lifetime
- 42 million Americans report that pain interrupts their sleep several times a week
Selecting a pain management physician
- Board certified/board eligible in pain management
- Fellowship trained pain management from an ACGME accredited program
- Background in anesthesiology, PM&R or neurology
- Well versed with ISIS & ASIPP guidelines
- Well versed with overall literature
- Extremely good hands and exceptional bedside manner
- Should be conservative in nature when treating patients and have a multidisciplinary approach in mind