Implanted Device Stimulates Nerves and Alleviates Pain
Treating Acute Nerve Pain With Electric Zaps
Published January 2024
Night and day. That’s how Brenda Sharp describes the difference between before and after getting a spinal cord stimulator implanted to help her manage her debilitating pain — thanks to the medical team at Northwestern Medicine Center for Pain and Spine Health Bloomingdale. Based on that success, the 50-year-old Kirkland, Illinois, resident was able to return to work and can now do the things she loves. She is full of energy and is no longer taking opioids to treat nerve damage in her spine.
Following two back surgeries in less than three years, Brenda remained in so much pain she could no longer play with her granddaughter, let alone stand for the 12 hours that her job as a respiratory therapist required. She tried a desk job, but the nerve pain would shoot down her leg, leaving her miserable and unable to concentrate. High doses of opioids and nerve medications did little to help the pain and left her in a constant groggy state.
The impact has been all positive. It is like night and day!— Brenda Sharp, Patient
“I couldn’t stand to be touched because the nerves were firing,” says Brenda. “I’m a half-glass-full type of person, but I was so depressed by the pain that I didn’t even leave my house. I had to stop working.”
Brenda’s surgeon referred her to Mehul P. Sekhadia, DO, a pain medicine specialist at Bloomingdale Center for Pain and Spine Health. Her surgeries had taken pressure off the nerve root, but the nerve was permanently damaged, causing chronic pain.
Alleviating the Pain With Technology
“Spinal cord stimulation was a great option for Brenda because it interrupts damaged nerve signals focally rather than systemically or at the brain level,” says Dr. Sekhadia. “All oral medications ultimately cross the blood-brain barrier and may cause unwanted side effects, such as cognitive or thinking difficulties, drowsiness or constipation.”

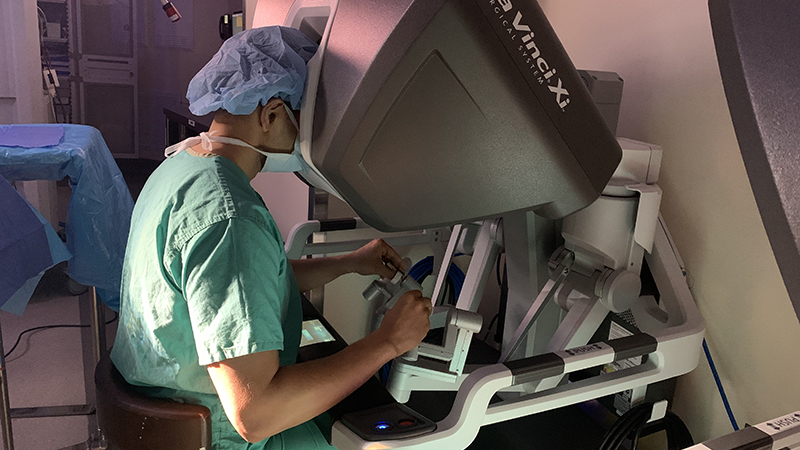
Bluetooth technology at Northwestern Medicine Center for
Pain and Spine Health Bloomingdale.
A spinal cord stimulator is a device similar to a pacemaker. A surgical team implants it just below the skin, typically in the back just above the hip. The device delivers mild electrical impulses to the spine through small wires called leads. The electric current blocks pain signals from reaching the brain.
“The spinal cord stimulators have evolved significantly over the past 50 years from a hardware perspective. Most importantly is our understanding of the technology and the various programming algorithms to minimize unwanted stimulation side effects,” Dr. Sekhadia says. “It is our current understanding that a damaged nerve signal is the source of many chronic pain conditions such as persistent sciatic pain, back pain after surgery or injury, or diabetic neuropathy.”
Stimulating the spinal cord (a process called neuromodulation) creates an energy field near the damaged nerve to interrupt its signals without affecting other areas of the body, most importantly the brain.
“Recent advancements in spinal cord stimulators have been amazing. There are patterns and adjustments that can be customized for every person to help reduce side effects and deliver more reliability,” says Steven R. Stakenas, APRN, an orthopaedic certified nurse practitioner at Bloomingdale Center for Pain and Spine Health. “We are excited about the next generation of stimulators, which will offer biofeedback to tell us how the nerve is responding.”
Enjoying Life Pain-Free
Within a few weeks of having the stimulator implanted, Brenda stopped taking the narcotic medications she had been on for years. She was also on a very high dose of the nerve medication gabapentin, which caused her to feel continuously drowsy and often fall asleep throughout the day. As she is slowly weaned off that medication, she visits the clinic monthly to adjust the neurostimulator using Bluetooth technology.
“Ten months after the procedure, Brenda is a completely different person,” Stakenas says. “She is full of life.”
Brenda returned to work as a respiratory therapist and often puts in overtime. She is most excited about the quality time she can now spend with her 6-year-old granddaughter and daily walks with her goldendoodle puppy.
“Before I had the neurostimulator implant, I was against it. I was in a really dark place because I was in so much pain, and I worried it would make things worse,” Brenda says. “But my advice to others in pain is to go for it. The impact has been all positive. It is like night and day!”