Care Team Performs 1st Robotic Lung Transplant in Illinois
Minimally Invasive Surgery May Cut Recovery Time in Half for Some Patients
Published February 2026
In a big step for lung care, surgeons at Northwestern Medicine did the first robotic lung transplant in Illinois. This breakthrough offers another option to some patients with advanced lung disease who may benefit from a less invasive surgical procedure.
For many people, a lung transplant can be lifesaving — but traditional surgery is complex and demanding on the body. Robotic technology may help reduce that burden for select patients.
How Robotic Lung Transplant Surgery Works
In a traditional lung transplant, surgeons must cut through the breastbone and open the chest wide to reach the lungs. This type of open-chest surgery can take eight to 10 hours and often leads to significant pain and a long recovery.
“A conventional lung transplant, where we cut through the breastbone and ultimately put it back together, is perhaps the most invasive, complex procedure performed at any hospital,” says Ankit Bharat, MD, chief of Thoracic Surgery and director of Canning Thoracic Institute, who performed the transplant. “We must open the chest like the hood of a car, so we have full access to the engine (lungs).”
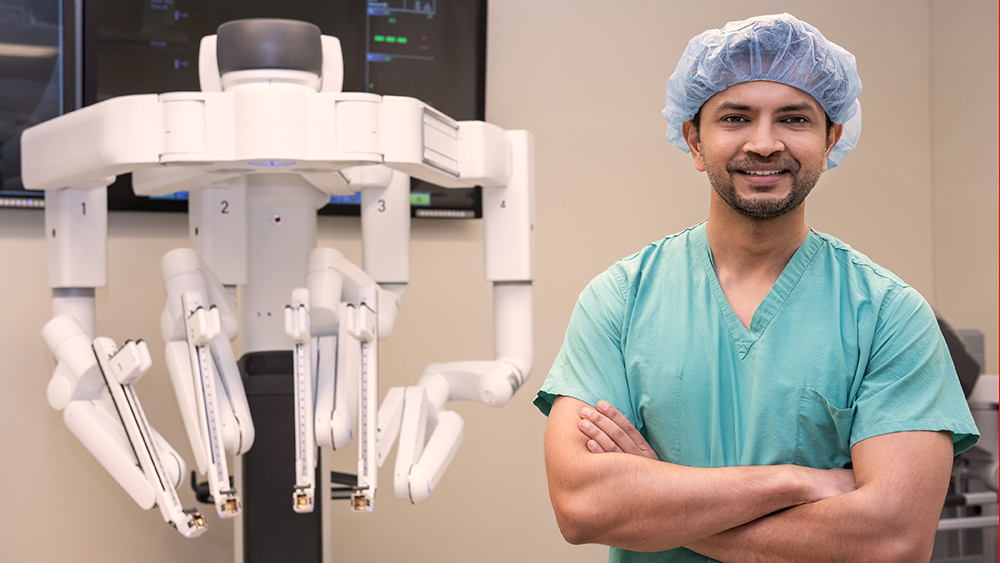
With robotic lung transplant surgery, surgeons use small incisions and robotic instruments instead. Doctors at Northwestern Medicine Canning Thoracic Institute used this approach to perform the entire transplant through small incisions on each side of the chest.
“A robotic approach allows us to dramatically reduce the invasiveness of the procedure, and we hope it will cut down on the recovery time for patients,” says Dr. Bharat.
Why Precision Matters in Lung Transplant Surgery
Robotic surgery allows surgeons to operate with high-definition, 3D views of the chest while controlling robotic arms from a console. These arms can move with incredible accuracy through four to five small incisions on each side of the chest.
This level of precision is especially helpful during lung transplant surgery, which requires extreme care and accuracy.
“The precision we achieve with robotic surgery is remarkable. We can perform incredibly complex maneuvers in tight spaces that human hands simply cannot access as effectively,” says Samuel S. Kim, MD, thoracic surgeon and director of Robotic Thoracic Surgery at Canning Thoracic Institute. He performed the procedure with Dr. Bharat.
“While more long-term data is still needed, we believe recovery time for these patients will be cut in half because they’ll have less post-operative discomfort,” adds Dr. Kim. “Robotic surgery is rapidly evolving, especially in the field of thoracic surgery, and we believe there’s a clear role for lung transplantation in carefully selected patients.”
A Patient Breathes Easier
The first robotic lung transplant in Illinois was performed on a man in his 60s with chronic obstructive pulmonary disease (COPD). COPD is a group of progressive lung diseases that obstruct airflow and make it harder to breathe. More than 17 million Americans live with COPD.
There’s currently no cure, but the disease is treatable. For this patient, a minimally invasive robotic lung transplant was a treatment option. Following the procedure, he was discharged from the hospital and is recovering well.
Who May Be a Candidate for Robotic Lung Transplant?
Robotic lung transplant surgery is not a good fit for everyone. Because of the high risks involved, patients are carefully screened.
This approach may be a good option if:
- You have emphysema or lung fibrosis
- You have larger chest cavities
- You have no prior chest surgeries
- You have stable heart function
- Your body type works well with robotic tools
“Every lung transplant carries life-or-death stakes with zero margin for error. We carefully select patients where robotics offers clear advantages without compromising safety or speed,” says Dr. Kim. “I don’t think robotic lung transplant will completely replace conventional lung transplant, but I do think it will become more popular in the future.”
Northwestern Medicine has a long history of advancing minimally invasive thoracic surgery, which helped make robotic lung transplants possible.

“At Canning Thoracic Institute, we have pioneered several transformative minimally invasive thoracic procedures, such as the robotic lung volume reduction surgery for emphysema, A-PLUS program for lung cancer, robotic SAINT program for advanced stage lung cancer and the robotic PREMIER program for esophageal cancer,” says Dr. Bharat. “So, developing a robotic lung transplant program was quite easy for us.”
Building on the Nation’s Leading Lung Transplant Program
The Lung Transplant Program at Northwestern Medicine is one of the busiest and most experienced in the United States. In 2024, the program performed 148 lung transplants. This was more than any other hospital in the U.S., with an average wait time of four days.
Since 2014, the program has completed more than 600 lung transplants and led national innovations. These include the first COVID-19 lung transplants in the country and the DREAM (Double lung transplant REgistry Aimed for lung-limited Malignancies) program for patients with advanced lung cancer.