Vaping ‘Was Silently Killing Me’
Published December 2019
Victory Over Vaping-Related Lung Injury
Allison had been smoking for 28 years on and off. Her fast-paced career in TV advertising lent itself to the buzz of nicotine. When vaping became widely available, she figured she could finally put out cigarettes for good at age 43. She vaped nicotine for about one year. After cannabis was legalized in Las Vegas, she started also vaping tetrahydrocannabinol (THC), the psychoactive component of marijuana responsible for a “high.” For the first time in years, Allison breathed easy. Little did she know that in two years, she would be struggling for air.
“With vaping, I could get rid of that horrible smell and taste of cigarette smoke and the constant need to go outside,” says Allison. “When I started vaping, my journey to better health, a better life and a better me seemed to be working.”
Allison’s skin got better. Her chronic cough dissipated. Her lungs felt like they could outlast her body. The burning sensation in her chest was gone. Her dentist even noticed that her gums were getting better.
“All signs pointed to vaping being a great thing for me,” says Allison. “What I didn’t know is that it was silently killing me.”
Fighting for Air
It started with chills and night sweats. It progressed into a high fever and vomiting.
“I believed I had influenza of some form,” says Allison. “Normally, I would have stayed home and waited it out, but a nagging concern about vaping because of the stories I was hearing in the news brought me into the Northwestern Medicine Emergency Department.”
Allison wouldn’t return home from the hospital for 10 days. “During that time, I was fighting for my life,” she says.
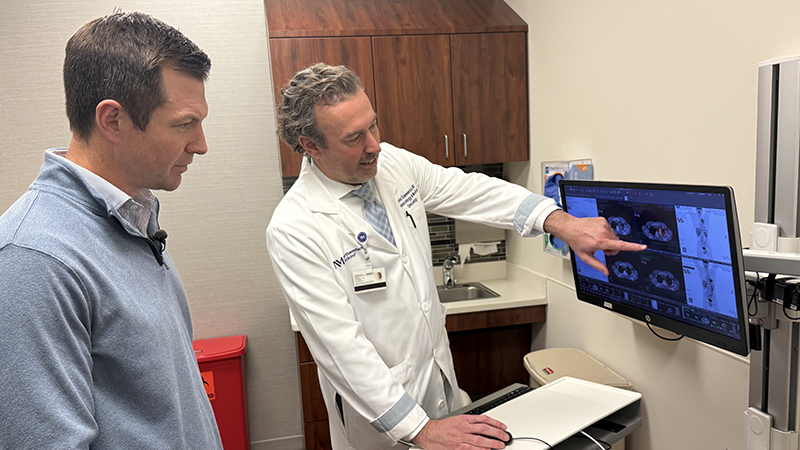
Was it the flu? Testing ruled out influenza, strep or other bacterial infection. Pneumonia seemed more like it, but Allison’s symptoms progressed. Her oxygen levels continued to decline. She struggled to breathe. She was transferred to the Intensive Care Unit and into the care of Northwestern Medicine Pulmonologist Khalilah L. Gates, MD.
“I was very concerned about Allison,” says Dr. Gates. “We worked hard to rule out all other potential causes of her lung inflammation before reaching the diagnosis: Vaping-related lung injury.”
Vaping-related lung injury is a “diagnosis of exclusion.” Because many of its symptoms are so similar to those of influenza, physicians must take a detailed patient history and rule out all other potential causes of the symptoms — shortness of breath, inflammation in the lungs, gastrointestinal distress, fever and cough — before moving forward with treatment.
Allison’s care team had their marching orders for her treatment. Her nurses stayed with her day and night to make sure she was breathing so they could avoid having to place her on a breathing machine. She was started on high doses of steroids to reduce the life-threatening inflammation in her lungs.
“I couldn’t make my lungs work, and I was terrified,” says Allison. “The feeling of not being able to breathe, to get oxygen, is something I can’t explain, but that no one wants to experience.”
Allison came off oxygen and returned home after more than a week in the hospital. Ten days later, she saw Northwestern Medicine Pulmonologist Clara J. Schroedl, MD.
“Steroids reduce inflammation, and thus far patients can recover quickly from vaping-related lung injury once starting treatment and refraining from vaping,” says Dr. Schroedl. “Recovery is challenging. However, the hardest and most important conversation I have with patients with vaping-related lung injury is how to make sure they can quit vaping for good.”
The Next Battle: Quitting
Vaping products have not been approved by the Food and Drug Administration as smoking cessation tools.
“It’s not safe to inhale anything into the lungs besides air,” says Dr. Schroedl. “Inhaling a burning chemical, additive or oil into the lungs is very dangerous.”
Allison adds, “I thought that I was giving up something bad and replacing it with something better. I truly believed vaping was safer than smoking, but one hit of a vape and I’d be right back in the hospital.”
It’s not safe to inhale anything into the lungs besides air.— Clara J. Schroedl, MD
It can be very challenging to break the vaping or smoking habit but your physician can help.