



The Root of Her Pain
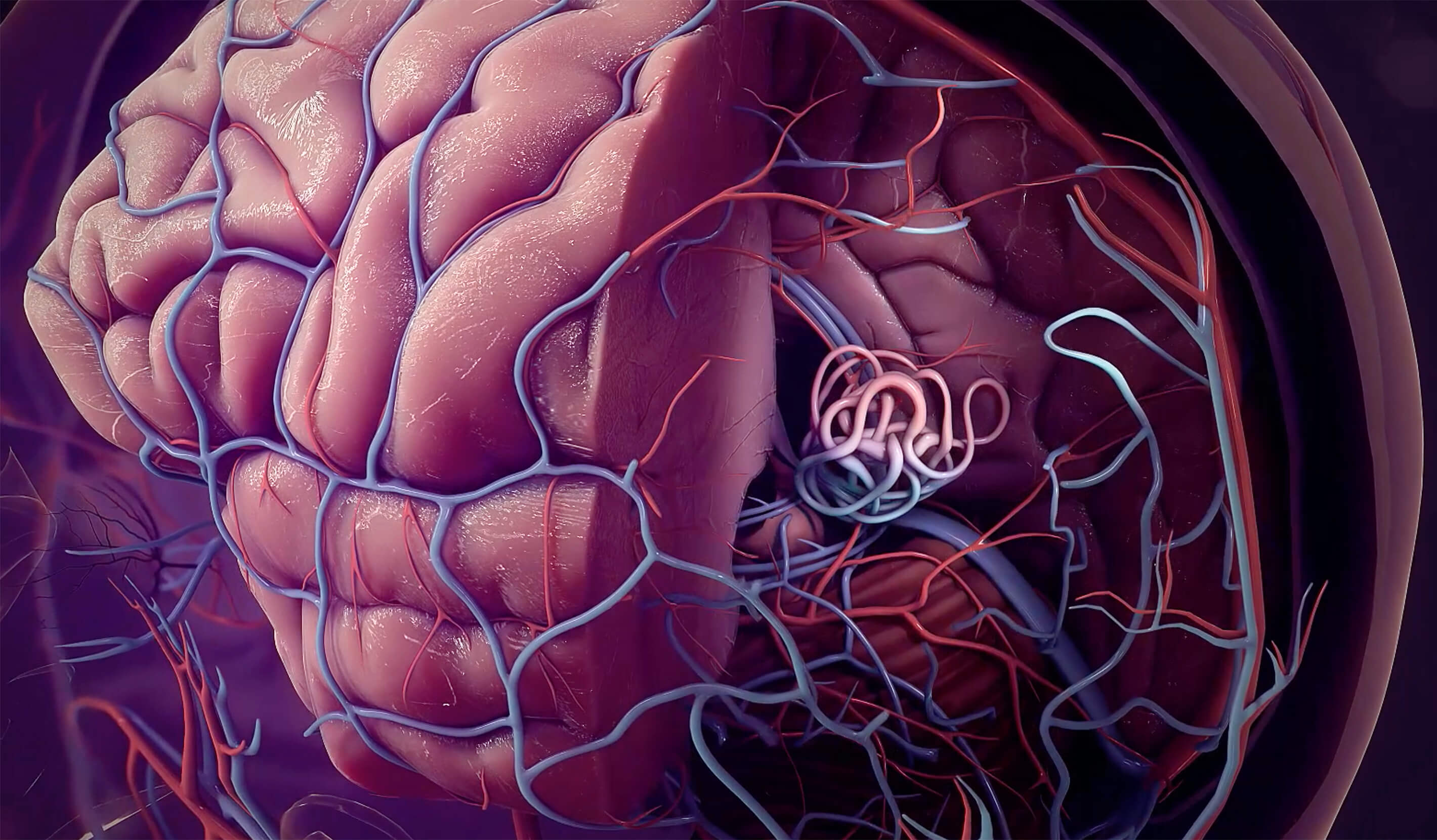
Imaging by her neurointerventional radiology team revealed that for Terrah, a second, more fatal brain hemorrhage wasn’t a matter of if, but when. She was suffering from a ruptured AVM. Terrah’s condition had likely existed since birth and was finally making its presence known.
It’s like a writhing, abnormal bowl of angry snakes rapidly shunting high-pressure blood into delicate veins.
Recognizing the urgency of Terrah’s condition, Neurological Surgeon Babak S. Jahromi, MD, PhD, sent an email with an unusual request to Cardiac Electrophysiologist Bradley Knight, MD. At February 4, 2019, at 3:02 pm, he messaged that he needed a “heart stopper,” a physician capable of disrupting the heart’s natural rhythm during surgery. Five minutes later, Dr. Knight responded in the affirmative. After Anesthesiologist Ljuba Stojiljkovic, MD, PhD, was also enlisted, Terrah’s care team was complete. What they were about to do was unprecedented.






What makes us better, makes you better.®

A Heartwarming Reunion
When you’re a mother and a wife, the thought of being separated from your family is devastating. And though her surgery improved her physical health, nothing felt better to Terrah than being back home with her husband, son and daughter.
I believed I was in the best hands. That was the reason that we chose to go to Northwestern Medicine.
The successful operation reinforced a fundamental tenet of the Northwestern Medicine approach to care — better collaboration leads to better patient outcomes. Now back on her feet, it’s almost as though Terrah never missed a beat.
One of the unique features of Northwestern Medicine is that you have leading experts in every field. And if you put them together, you can get amazing results.