What to Eat (and Avoid) During a Diverticulitis Flare-Up
Your Diet Matters
Published July 2025
When you’re having a diverticulitis flare-up, one of the most important things you can do is watch what you eat. Certain foods can help your body heal, while others can make symptoms worse.
What Is a Diverticulitis Flare-Up?
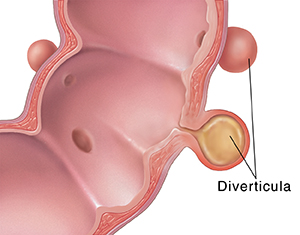
To understand diverticulitis, it helps to start with diverticulosis. Diverticulosis happens when small pouches, called diverticula, form in the lining of your colon (large intestine). These pouches are quite common, especially after age 40, and often cause no symptoms — most people with them don’t even know they have them. In fact, more than half of people in the United States over the age of 60 have diverticula. Diverticulitis happens when these pouches become inflamed, typically from a tear or bacterial infection. This can cause:
- Stomach pain (often in the lower left side)
- Tenderness in your stomach area when touched
- Bloating
- Fever
- Nausea
- Constipation or diarrhea
When these symptoms happen, it’s called a flare-up. Your colon needs rest, and the right foods can make a difference.
According to David M. Manuel, MD, a gastroenterologist at Northwestern Medicine, “The incidence of diverticulitis is increasing with the largest increase in patients aged 18 to 44. This rising number of cases in young adults is a strong reminder that taking care of your digestive health is important at every age.”
Dr. Manuel notes that in addition to diet, other lifestyle factors, including a lack of physical activity, obesity, smoking and heavy alcohol use, can increase your risk of diverticulitis.
What to Eat
During a flare-up, your care team may recommend a special diet to reduce irritation and inflammation and to help your gut heal. This can be a clear liquid or low-fiber diet. Always consult with your physician or a registered dietitian before starting any restrictive diet, especially for medical conditions. They can provide guidance and ensure that your nutritional needs are met.
Clear Liquid Diet
If your flare-up is severe with persistent diarrhea, fever or pain, or you need surgery, you may be placed on a clear liquid diet. This typically includes:
- Water
- Sports drinks, also known as electrolyte drinks
- Clear broth (chicken, vegetable or beef)
- Fruit drinks without pulp or fruit pieces, like filtered apple juice, cranberry juice or grape juice
- Plain or flavored gelatin
- Frozen juice bars made from clear juices without pulp or fruit pieces
- Hot or cold coffee or tea with no milk or creamers
“When someone is acutely flaring, they are often given the suggestion to go to a clear liquid or low-fiber diet,” says Bethany M. Doerfler, MS, RDN, a clinical research dietitian at Northwestern Medicine Digestive Health Institute. “This is really to help make you comfortable and not to suggest that fiber is dangerous.”
Low-Fiber, Soft Food Diet
If your symptoms are mild or improve after a clear liquid diet, your care team may recommend foods that are soft and easy to digest. These foods may be chopped, ground, mashed or pureed to make them gentler on your digestive system.
Grains
- White bread
- Unsalted white crackers
- White rice
- Pasta
- Low-fiber cereals such as puffed rice or cream of wheat
Fruits
- Applesauce
- Bananas
- Cooked or canned fruits without skin or seeds
- Smoothies without seeds or fruit pieces
- 100% fruit juice with no pulp
Vegetables
- Cooked or mashed vegetables without skins, stems or seeds
- 100% vegetable juice with no pulp
Proteins
- Skinless fish, turkey and chicken
- Eggs
- Tofu
- Smooth peanut butter and other nut butters
- Ready-to-drink protein shakes
Dairy (if tolerated)
- Milk
- Cottage cheese, soft cheeses
- Yogurt, including Greek yogurt, kefir and yogurt drinks without seeds or fruit pieces
“Opting for foods like mashed potatoes, egg or tuna salad, or pureed sweet potatoes is a popular way to modify fiber and improve your tolerance,” says Doerfler.
Regarding whether probiotics can provide symptom relief, Doerfler says, “No studies to date have been able to show probiotic supplementation can shorten a flare.”
Foods to Avoid
The following foods are hard to digest or promote inflammation, which can worsen symptoms during a flare:
- Fried or greasy foods
- Spicy foods
- Red meat and processed meats
- Alcohol
- Pastries, candy, sodas and other foods high in refined sugar
It is important to note that individual responses to food can vary. Consider keeping a food diary during a flare-up to help you and your care team identify any specific foods that trigger symptoms for you.
A Return to High-Fiber Foods
Once your flare-up is fully over (usually in a week or two), you should gradually return to a high-fiber diet, which can help prevent future flare-ups. A high-fiber diet keeps your poop soft, promotes regular bowel movements and reduces pressure on your colon, which is thought to lower the risk of diverticula forming and becoming inflamed.
Aim for 25 to 35 grams of fiber daily, gradually increasing to avoid bloating and discomfort. Be sure to drink plenty of water for fiber to work effectively, and avoid or quit smoking, which can damage your colon wall.
Good fiber sources:
- Whole grains such as brown rice, oats, whole wheat bread and quinoa
- Whole or dried fruits such as apples, apricots, berries, figs, mangos, oranges, pears and plums
- Raw vegetables such as leafy greens, broccoli and carrots
- Beans, peas and lentils
- High-fiber cereals
“A healthy eating pattern providing a diet rich in fiber from whole foods, limited in refined sugars and alcohol, is the best eating pattern to reduce the risk of future flare-ups,” says Doerfler.
The Shift on Nuts, Seeds and Popcorn
Previously it was common for medical professionals to advise patients with diverticulosis or a history of diverticulitis to avoid small, hard foods like nuts, seeds, corn and popcorn. The theory was that these foods could get stuck in the diverticula, leading to inflammation or infection and triggering a diverticulitis flare-up.
“Nutritional science no longer suggests that people need to avoid nuts, seeds or popcorn,” says Doerfler. “These fibrous foods can be enjoyed even if you are flaring but you need to make sure you are chewing them well. Additionally, nut butters, such as walnut, almond or peanut butter, provide texture-modified ways to consume nuts even if you are temporarily reducing fiber.”
The current understanding emphasizes a high-fiber diet for long-term management and prevention of diverticulitis, and a temporary low-fiber or clear liquid diet during an acute (severe) flare-up to allow your colon to heal. You may need antibiotics or other treatment to prevent complications.
Learn more about eating for colon health.