Innovative Treatment Saves Patient With Stage 3 Lung Cancer
Genetic Makeup of Tumor Guides Plan
Published October 2025
Kathie Schultz, 63, of Union, Illinois, went to the emergency department thinking she had a bad upper respiratory infection. Tests revealed something much worse: stage 3 lung cancer.
Kathie’s care team at Northwestern Medicine McHenry Hospital went into action to develop an innovative plan that included genetic analysis, pre-surgical treatment and a high-precision robot to remove her entire left lung. After surgery, Kathie returned home cancer-free.
Next-Generation Sequencing: The Customized Approach
Before she underwent robot-assisted surgery, Kathie’s oncology team used next-generation sequencing, a technology for determining DNA sequencing to identify errors or mutations that may be associated with diseases, such as cancer. This detailed genetic information allows physicians to develop customized treatments.
With next-generation sequencing, Kathie’s oncology team was able to get an understanding of how Kathie’s tumor behaved and how to approach the systemic treatment of it. Based on this, they administered both chemotherapy and immunotherapy before surgery to reduce the size of Kathie’s tumor. It worked. Kathie’s tumor size went from a little over 9 centimeters (cm) to 4 cm at the time of surgery.
“What’s novel about Kathie’s case is using a treatment customized for her based on the genetic makeup of her tumor. We could first shrink the tumor to the point that it could all be removed, and we could cure her,” says Ankit Bharat, MD, an oncologist at Northwestern Medicine who was part of Kathie’s care team. “Prior to giving that therapy, the tumor was not completely removable. Although surgical removal of the lung is a highly complex procedure — especially in patients who have received chemotherapy and immunotherapy — we are happy that we could do this for Kathie using the most advanced minimally invasive robotic approach.”
The Benefits of Robot-Assisted Lung Removal
Because Kathie’s surgery was robot-assisted, surgeons were able to use a minimally invasive technique, which significantly shortened her recovery time. Kathie’s largest incision was less than an inch and a half, and surgeons did not have to cut through bone or muscle. She spent three days in the hospital after surgery — about half the typical duration — with minimal discomfort.
“It was amazing,” says Kathie. “I was shocked. The scar is like non-existent after eight weeks. This team saved my life, and because of them, I am cancer-free.”
The Importance of Lung Cancer Screenings
Before her surgery, Kathie smoked and had never received a screening for lung cancer. She says she’s sharing her story to emphasize the importance of lung cancer screening.
The American Cancer Society updated its lung cancer screening guidelines in late 2023, broadening the scope of recommended testing. They recommend yearly screening for lung cancer for:
- People aged 50 to 80 who currently smoke
- People who used to smoke with a 20-year or greater pack-year history
- To determine pack-years, multiply the number of packs per day smoked by the number of years you smoked.
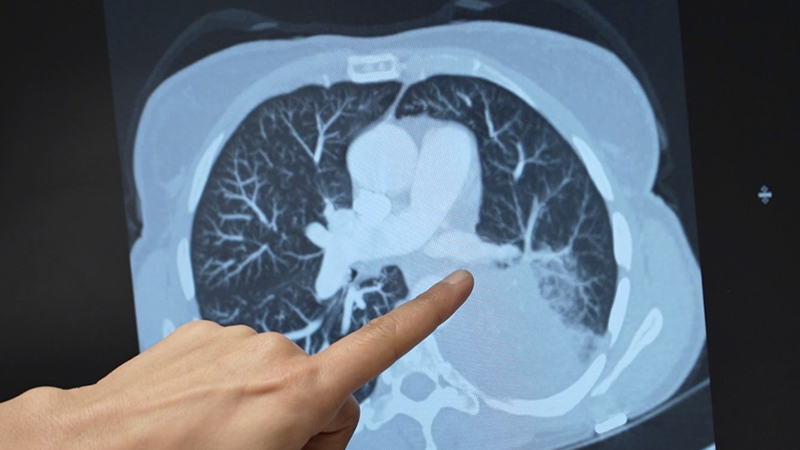
The recommended annual screening test for lung cancer is a low-dose computed tomography scan, also called a low-dose CT scan or LDCT.
“Don’t wait until you feel terrible,” says Kathie. “I mean, everybody feels great until they don’t. And when that happens, it’s such a shock. If I could encourage even one person to get screened, that’s all I could ever ask for. I was just so lucky.”