2 Hearts at Stake
Published September 2021
The Complex Surgery that Saved Jessica and Her Baby
There's a phrase in medicine: "When you hear hoofbeats, think horses not zebras." This means that when diagnosing a patient, physicians start with the most common cause of the symptoms rather than the rarest one.
When she was 29 weeks pregnant, Jessica Moore was short of breath to the point of needing a walker to get around. Her Northwestern Medicine OB/GYN sent her to the Emergency Department at Northwestern Memorial Hospital.
Every day made a difference.— Shilajit D. Kundu, MD
The cause of her shortness of breath was not a horse but a zebra: a tumor growing out of her heart.

is the tumor growing out of Jessica's heart.
A scan found a 9-centimeter tumor thrombus, or fingerlike extension, growing from Jessica's inferior vena cava, the largest vein in the body that comes out of the back of the heart. The inferior vena cava brings blood from the lower body, pelvis and abdomen to the heart to be pumped into the lungs for oxygenation.
"Jessica's tumor was near a lot of critical structures, including her liver and kidneys," says Northwestern Medicine and Robert H. Lurie Comprehensive Cancer Center of Northwestern University Sarcoma Surgeon Jeffrey D. Wayne, MD. "It was an imminent threat to her health and to her baby, who was not yet mature enough to deliver."
To determine what they were up against, Jessica's care team had to do a biopsy of the tumor, which was not exactly in the most accessible location. Since Jessica was also 29 weeks pregnant, she couldn't be put under anesthesia. Jessica remained awake while her team threaded a catheter with a claw on the end of it through an artery in her groin up to her heart to grab a tissue sample from the tumor. When the biopsy results indicated sarcoma, a cancer of the soft tissues, the physicians on Jessica's team didn't think twice. They started planning the fight to save mom and baby.
The Simple Answer
"If we gave her chemotherapy, we would give her not very long to live," says Dr. Wayne. "The simple answer was surgery. It was high risk but high reward for Jessica, who was a young and strong mother and wife."
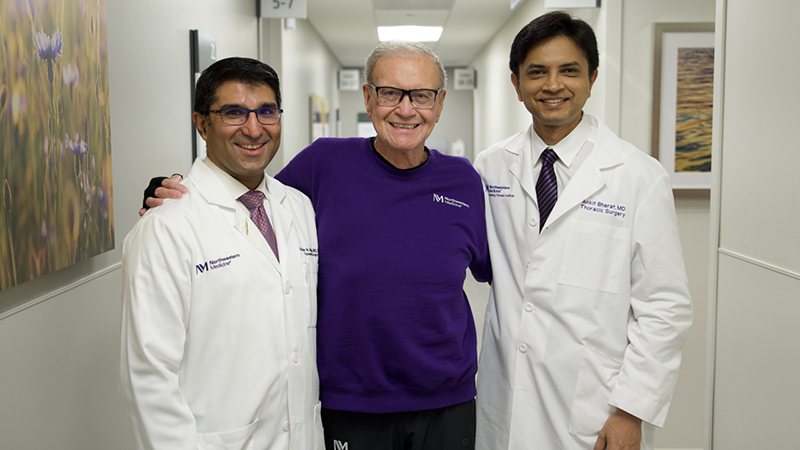
Jessica had a rare tumor, but luckily she also had rare team of experts with experience in these types of cases.
But before the surgery could happen, they had to wait for Jessica's baby to become mature enough to be delivered. They waited 10 days so that Jessica would be at the 31-week point and be capable of having a safe and healthy C-section. During those 10 days, her tumor grew 4 centimeters.
"That's when we realized the urgency of this case. A patient can die from a rapidly progressing tumor thrombosis," says Northwestern Medicine and Lurie Cancer Center Urologic Oncologist Shilajit D. Kundu, MD. Dr. Kundu and his team took the lead on Jessica's case. "Every day made a difference, and there were two hearts at stake."
The high-risk maternal fetal medicine team, led by Northwestern Medicine Maternal Fetal Medicine Physician Nevert Badredin, MD, delivered baby Julia. Though healthy, she had to spend some time in the Neonatal Intensive Care Unit due do her premature delivery. A few days later, Jessica went into a 10-hour surgery to remove the tumor in her heart.
A Complex Surgery
Jessica's team, led by Dr. Kundu, made a plan and never looked back. Jessica's surgical team consisted of:
- Dr. Kundu
- Northwestern Medicine Vascular Surgeon Mark K. Eskandari, MD
- Northwestern Medicine Transplant Surgeon Juan Carlos Caicedo, MD
- Northwestern Medicine Cardiac Surgeon Duc Thinh Pham, MD
For cases like Jessica's, the size of the tumor is not the concern. The concern is the location. Jessica's tumor was in one of the trickiest areas of the body. Any nick or misstep could result in significant and unrecoverable hemorrhage. Tumor thromboses also have "clotting factors" on the end of them. These clotting factors can easily break off and travel to the heart or lungs. If this happened, there was a chance that Jessica could die instantly in the operating room. That's why her surgical team took a methodical, step-by-step approach.
"We made a plan, and everyone executed their part flawlessly," says Dr. Wayne.
Step 1: Put the Heart on Bypass
Because the tumor was growing into Jessica's heart, her team had to put Jessica on cardiopulmonary bypass. A machine temporarily took over the function of her heart and lungs, circulating blood and oxygen throughout her body during the surgery.
Step 2: Mobilize the Liver and Kidneys
The inferior vena cava extends down into the liver. The tumor thrombus was "sticking its tongue" into the liver veins from the heart. To access the tumor in the inferior vena cava, Dr. Caicedo had to mobilize the liver and hold it outside of Jessica's body so that the team could access the tumor in her inferior vena cava. Dr. Kundu had to do the same with the kidneys. To do this, they also had to mobilize the retroperitoneum, the tissue that lines the abdominal walls and holds most abdominal organs in place. Dr. Caicedo helped "milk" the tumor thrombus out of the veins in the liver, being careful not to break off any clotting factors.
Step 3: Control the Vena Cava
Dr. Eskandari clamped Jessica's vena cava at the top. With the lower part of the tumor completely freed from the liver, the team carefully cut Jessica's vena cava in half and pulled the tumor out of it from below. They reconstructed her vena cava with a prosthetic vein made out of Gore-Tex® that Jessica will always have.
Step 4: Put Everything Back Together
With the tumor removed and Jessica's prosthetic vena cava in place, the team replaced her organs and took her off cardiac bypass.
"Without multidisciplinary involvement, this could not have been done," says Dr. Kundu. "Jessica is very lucky she ended up at one of the few hospitals willing to take a case like this. We were all willing to fight for her."
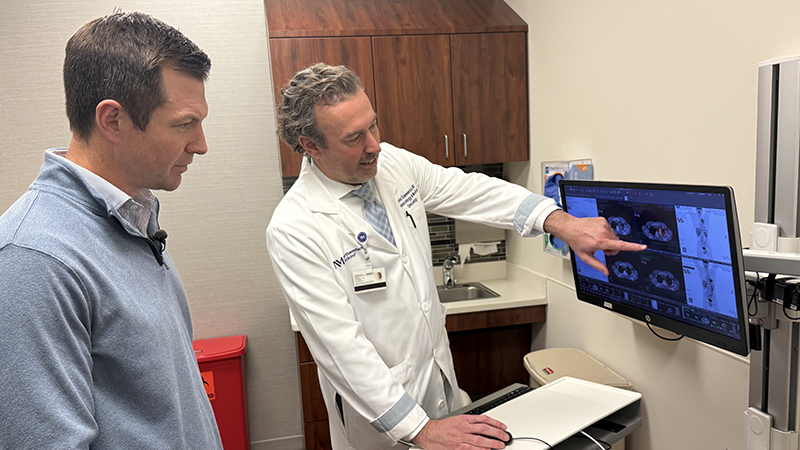
Jessica is now one year out from her operation and is grateful for every day with her husband and two children. She returns to Northwestern Medicine several times a year for scans to make sure she is still cancer-free. As for the team that saved her and Julia's life, Jessica says, "I'm beyond grateful to have ended up at the right hospital with the right team and at the right time."