A World-Class Cardiovascular Care Clinic for Veterans
Northwestern Medicine Cardiologist Opens Advanced Heart Failure Clinic at Jesse Brown Department of Veterans Affairs Medical Center
Published February 2024
Many veterans face healthcare challenges such as financial insecurity, housing instability, neighborhood crime and lack of access to transportation. These can all have a negative impact on their health. Veterans also often have high rates of diabetes, high blood pressure, obesity and heart failure.
To help address the needs of this population, Sarah E. Chuzi, MD, a cardiologist at Jesse Brown Department of Veterans Affairs Medical Center (Jesse Brown VAMC) and Northwestern Medicine Bluhm Cardiovascular Institute, established an advanced heart failure clinic for veterans at Jesse Brown VAMC. This collaboration is a continuation of a longstanding relationship between the two organizations. For more than 77 years, medical residents from Northwestern Medicine have rotated through the Jesse Brown VAMC during their medical training, the longest academic affiliation in the VA system.
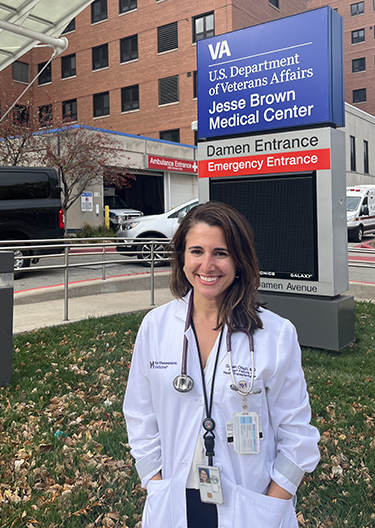
Dr. Chuzi credits her medical training at Jesse Brown VAMC as the inspiration for wanting to dedicate her career to caring for veterans.
“The VA has always had a special place in my heart. Mainly because of the patients, the veterans,” continues Dr. Chuzi, who has veterans in her own family. “They are so resilient and strong, and they have served our country. They are incredibly deserving of good care.”
Navy Vet Dwayne Patterson’s Story: From Heart Failure to Heart Transplant
Dwayne Patterson, 58, looks back on his time in the United States Navy with pride. The tours of service he was on gave him the opportunity to see the world — sending him everywhere from Hawaii to Australia, Singapore, the Philippines and more.
After serving in the Navy, Dwayne eventually returned to federal service, taking a job with the U.S. Postal Service. One day at work in Minnesota, Dwayne noticed changes in his health.
“It came on very suddenly. I was working in the mailroom and started feeling short of breath when walking just short distances from one side of the room to the other. I knew something was wrong,” explains Dwayne, who left work and drove to the nearest urgent care clinic.
After being told he needed a higher level of care, Dwayne drove himself to the emergency department at the nearest academic medical center in Minneapolis. He would not see the outside of a hospital again for three weeks.
“I lost consciousness in the ER that night. When I woke up the next morning, they told me I had 13 TIAs, or miniature strokes, overnight,” says Dwayne. “The doctors told me that these were warning signs, and the big one would come if I didn’t seek treatment immediately.”
Dwayne’s health continued to decline. He spent the next two months in and out of the hospital, and was eventually diagnosed with congestive heart failure. His heart was functioning at less than 5% of its normal capacity. Dwayne’s best option for survival would be a heart transplant or left ventricular assist device (LVAD).
Finding Support and Care in Chicago
Dwayne made the decision to seek care in Chicago where he had family support from his sister. They drove from Minnesota directly to the Jesse Brown VAMC where he met Dr. Chuzi.
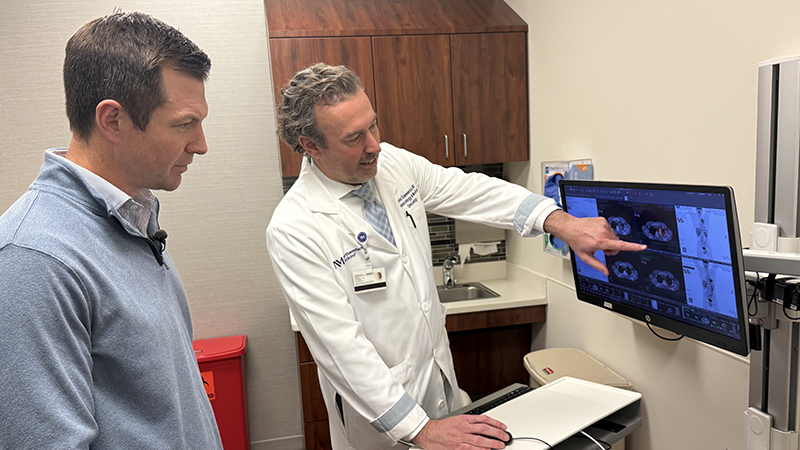
“Dwayne got sick very quickly. When I first saw him in clinic, he could barely get onto the exam table without shortness of breath,” says Dr. Chuzi. “If you have taken care of a veteran, or met a veteran, you know that they are very stoic, and they are unlikely to complain. So, I knew, just looking in his eyes, that he was very sick and really scared, and that he needed an intervention quickly.”
We hope this program will help veterans get the care they need.— Sarah E. Chuzi, MD
Dr. Chuzi and a multidisciplinary team of Northwestern Medicine and VA clinicians began the process of evaluating Dwayne for a heart transplant. He was too sick to go home, so he was admitted to Northwestern Memorial Hospital to wait for a donor heart, which came a month later in April 2023.
“I remember the day the call came. I was in the hospital and not feeling well, then they told me, ‘We found you a heart and we want to schedule surgery,’” says Dwayne. “You know, I never feared. I’m a man of faith, which guided me. I knew I had the best medical team at one of the best hospitals for a heart transplant and at the VA. I was ready.”
Following his transplant, Dwayne faced some initial challenges adapting to life with his new heart. But today he is feeling better than he has in years. He has since retired from the Postal Service and is enjoying time reconnecting with his friends and family in the Chicago area. His heart donor and their family are never far from his mind.
“Like my sister says, someone died for you to live. So, I always keep that in the back of my mind,” says Dwayne. “I would just say thank you for this blessing. I have a second chance at life now.”
“Heart failure in general is extremely burdensome to the population at large, but especially to our veterans because the risk factors for heart failure are so prevalent,” says Dr. Chuzi. “This is a population where there is a ton of advanced disease, but if you don’t have someone who is specifically trained in looking for patients with this disease, you might not find it. We hope this program will help veterans get the care they need.”
In less than a year, more than 10 patients have been referred to Northwestern Medicine from the Jesse Brown VAMC for advanced heart failure surgical therapies, with eight patients receiving LVADs in just six months.