What Is Targeted Muscle Reinnervation (TMR)? [Infographic]
Amputation Nerve Pain Relief
Published August 2023
Medical advances in the field of prosthetics have brought improved quality of life for individuals with limb loss. Among these advances is targeted muscle reinnervation (TMR).
This surgical procedure was pioneered in 2002 by Gregory A. Dumanian, MD, a plastic surgeon at Northwestern Medicine, and Todd Kuiken, MD, PhD, a physiatrist and professor at the Northwestern University McCormick School of Engineering. It was originally developed to help people who had limbs amputated control their upper limb prosthetics. In their research, Dr. Dumanian and Dr. Kuiken observed an unexpected benefit of TMS surgery: reduced phantom limb pain and neuroma.
Whenever you cut a nerve, it’s trying to heal.— Gregory A. Dumanian, MD
This is an important advance in care as a significant percentage — approximately half — of the 185,000 people who get new amputations in the U.S. each year experience moderate-to-severe chronic post-amputation pain.
Understanding Targeted Muscle Reinnervation
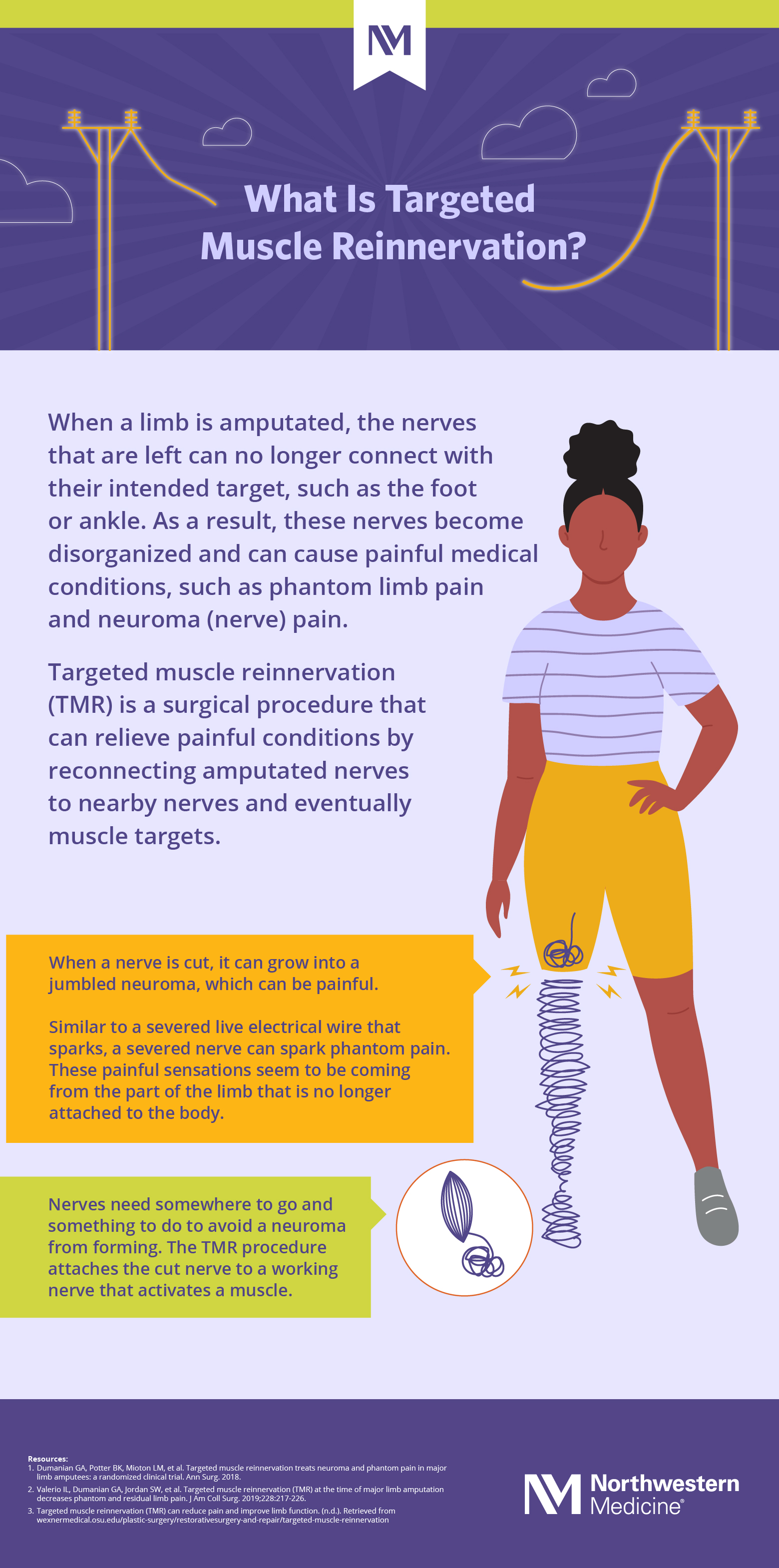
TMR is a surgical procedure that reroutes amputated peripheral nerves (nerves that branch out from the brain and spinal cord) by attaching them to nearby nerves that activate muscles.
“Whenever you cut a nerve, it’s trying to heal. It’s trying to find a home,” says Dr. Dumanian. “When a nerve is frustrated and it attempts to heal, it can grow to form a neuroma, which is a jumbled end of a nerve. Neuromas don't have a terminal receptor. They're not connected to anything.”
Dr. Dumanian explains that a severed nerve is similar to a live wire in electricity. The energy has no place to go, so it sparks, which can cause pain. “The jumbled end of the nerve can also send disorganized information back up to the brain,” he says. “Every brain interprets this information — or lack of normal information — differently.” For some people, the confused signals result in phantom pain, which are painful sensations that seem to be coming from the part of the limb that is no longer attached to the body.
The way to lessen, and in some cases stop, phantom and neuroma pain is to connect the broken nerve to a nearby nerve attached to a muscle. This gives the broken nerve somewhere to go and something to do, restoring normal signals to the brain.
Dr. Dumanian says neuroma can grow to be as large as a golf ball, but most are the size of a pea. And, not all neuroma are painful. Depending on the location of a neuroma, your physician can sometimes feel the firm nerve mass during an exam.
TMR Timing
TMR is most effective at the time of an amputation, says Dr. Dumanian, but it can also be performed years after an amputation if you are experiencing phantom pain or pain from a neuroma.
TMR Surgery: What to Expect
- A TMR surgery lasts about two to four hours, and typically requires you to stay overnight in the hospital for one to five days.
- Your physician will schedule follow-up appointments.
- If you had TMR at the time of amputation, you can begin the fitting process for your new prosthetic at six to eight weeks.
- If you had TMR for established nerve pain (after amputation), you may be back to work as early as three weeks after surgery, depending on the type of work you do.
- Most people experience surgery-related pain but not original nerve pain immediately after the TMR procedure. “The nerve can then ‘wake up’ after a period of time,” says Dr. Dumanian. “Nerve pain may increase while nerves grow and connect with new targets.”
- Your need for pain medication will decrease as the nerves heal. Over time, many people can reduce or eliminate the need for pain medications under their physician’s supervision.
When TMR Is Not an Option
You are not a candidate for TMR if:
- You have a spinal cord injury.
- You have a brachial plexus nerve root injury (injury to the roots of nerves that extend from the spinal cord and send signals to the shoulder, arm and hand).
- Your pain is from a pinched nerve. For example, carpal tunnel is a pinched nerve, and the treatment is decompression, not TMR.
- Your health does not meet the requirements for the surgery.
If you are living with chronic pain following an amputation or are planning an amputation, talk with your physician to determine if TMR is an option for you.
 Download What Is Targeted Muscle Reinnervation (TMR)? [Infographic]
Download What Is Targeted Muscle Reinnervation (TMR)? [Infographic]