The Anatomy of PPE [Infographic]
Published January 2022
Understanding Personal Protective Equipment
You may be hearing the term “PPE” more frequently since the onset of the COVID-19 pandemic, but personal protective equipment (PPE) is nothing new. In fact, it has existed for centuries to help keep patients and healthcare providers safe.
If you have COVID-19, you are capable of spreading the virus through respiratory droplets when you sneeze, cough and even just talk. The droplets can be breathed in by others, or can land on surfaces that other people touch. PPE creates a barrier to keep viral particles away from individuals who are not infected. That’s why wearing a face mask is essential in fighting the COVID-19 pandemic.
“Due to the current prevalence of COVID-19 in the community, anyone who enters our facility is currently required to wear a medical mask issued by Northwestern Medicine,” states Rachel Weber, infection preventionist at Northwestern Memorial Hospital. These masks are fluid-resistant and help form a barrier against infected droplets.
Face masks (procedural and surgical) are the most basic PPE required at Northwestern Medicine. However, there are different types of masks that filter out different-sized particles.
Staff are trained to protect themselves by wearing necessary PPE.— Rachel Weber, infection preventionist
Read on to learn about the more advanced PPE in use to protect patients, visitors and healthcare heroes at Northwestern Medicine.
- One size does not fit all. Not all providers will wear the same size or type of PPE. Gowns, for example, are sized to each provider to ensure there are no gaps. Additionally, different types of respirators — from N95 respirators to elastomeric respirators and powered air-purifying respirators (PAPR) — must be seal-checked to accurately fit each user. The fit test, which takes 15 to 20 minutes, evaluates the seal between each provider’s face and the respirator equipment’s facepiece to assign individual sizing, make and model for adequate protection. To remain accurate, the process is repeated on all providers at least once per year.
- Having PPE available is only the beginning. PPE won’t keep you safe if you don’t use it properly. Following guidelines from the Centers for Disease Control and Prevention (CDC), Northwestern Medicine ensures all healthcare providers have adequate PPE, but also provides training so they know how to properly put it on and remove it, a process called donning and doffing.
- It’s not all disposable. Some PPE can be reused if handled and cleaned adequately. For example, PAPR hoods may be worn continuously by the same person for a shift for multiple patients, and then disinfected and stored for reuse. Additionally, face shields and goggles can be reused if disinfected and in good condition, allowing for clear vision without any cracks or damage.
- PPE is not just for COVID-19. The Northwestern Medicine workforce is well trained in the use of PPE, so they were ready when the pandemic hit. “If there is an anticipated risk of exposure to contaminated bodily fluids during any treatment, staff are trained to protect themselves by wearing necessary PPE,” says Weber. During the pandemic, preventive measures are taken with all routine patient care. “When entering a patient’s room, all staff members wear surgical or procedural masks as well as eye protection.”
- Four types of PPE are necessary to treat patients who have COVID-19. Each item protects a different part of the body. Specific choices vary depending on the type of care provided.
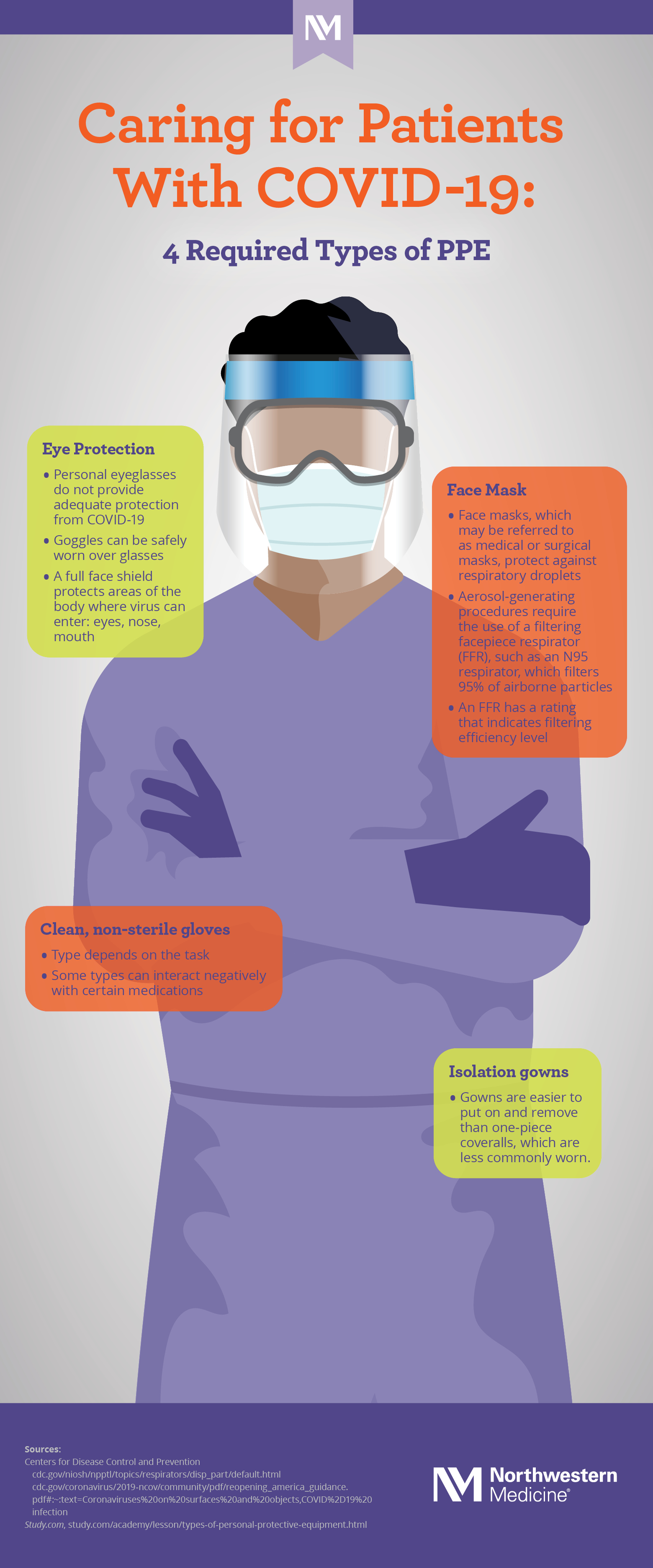 Download The Anatomy of PPE [Infographic]
Download The Anatomy of PPE [Infographic]